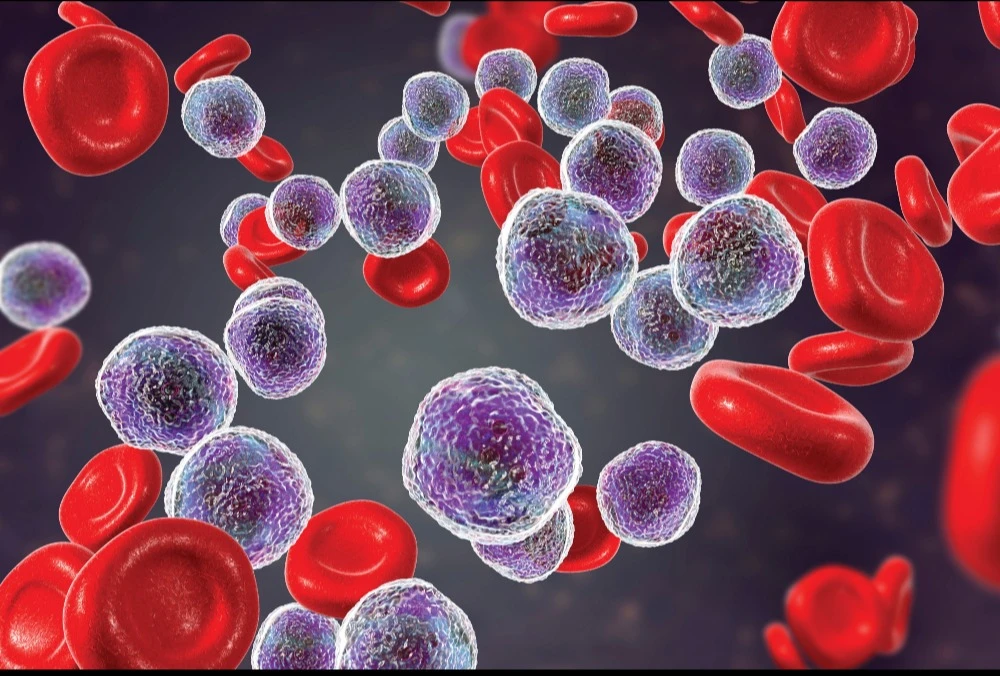
Chronic Lymphocytic Leukaemia (CLL)

Chronic Lymphocytic Leukaemia (CLL) is a type of blood cancer that starts from the lymphocytic white blood cells produced in the bone marrow. There is an overproduction of abnormal white blood cells, which crowds the bone marrow and prevents the production of normal blood cells.
A Leukaemia is acute or chronic depending on which blood cells is involved and thus, how quickly it grows. Acute leukaemias grow quickly when left untreated, while chronic leukaemias take more time to develop. Most people can live with chronic leukaemias for many years.
Although there are no proven causes for CLL, it is thought to arise from a mutation in the genes controlling blood cell development. Such mutations occur during a person’s lifetime and are not passed to the next generation. Certain risk factors for developing CLL have been identified:
- Age – The risk of developing CLL increases with age. CLL occurs most frequently in people over 60 years of age, and rarely in people under 40 years of age.
- Gender – CLL is more common in men than in women.
- Family history – First-degree relatives (parents, siblings or children) of a person with CLL may have a higher risk of developing CLL themselves.
- Ethnicity – People with relatives who are Eastern European Jews or Russian Jews have a higher risk of developing CLL.
- Exposure to chemical agents – People who were exposed to Agent Orange, a herbicide used during the Vietnam War, may have a higher risk of developing CLL.
CLL may cause only mild symptoms and many people may not experience any symptoms at all. CLL may even be discovered incidentally during a routine blood test. However, sometimes CLL can cause the following symptoms:
- Fatigue
- Fever
- Breathlessness
- Feeling weak
- Pale skin
- Loss of appetite
- Weight loss
- Night sweats or excessive sweating
- Bleeding gums or nosebleeds
- Bruising easily
- Red or purple spots on the skin
- Bone or joint pain
- Feeling of fullness in the stomach or swollen stomach
- Painless lumps in the neck, underarm, stomach or groin
- Frequent infections
A physical examination, blood test and bone marrow biopsy will help with diagnosing and prognosticating CLL.
In the physical examination, the doctor will check for general signs of health, and look for swelling in the liver, spleen and lymph nodes, unusual bleeding or bruising, and signs of infection.
The blood test, called a full blood count, involves a sample of blood being sent to the laboratory for investigation. The blood sample will be checked for the number of different blood cells. A high proportion of lymphocytes (over 5,000 lymphocytes/ mm3) along with low levels of red blood cells and platelets may indicate CLL. When examined under the microscope, a blood smear of a person with CLL may also show smudge cells, or abnormal-looking lymphocytes.
A bone marrow biopsy involves taking a sample of bone marrow, usually from the hip bone. This is done under local anaesthetic and takes 15 – 20 minutes. The sample will also be sent for investigation by the laboratory, to be examined for cancerous cells.
Flow cytometry is a test that uses a machine to help identify CLL cells in blood samples or bone marrow samples. Flow cytometry is the most important test used for diagnosing CLL.
Further tests, including blood test, chromosome analyses, and imaging tests (e.g. CT-scans) are usually also done to determine the extent of the CLL and to help determine the best treatment options.

There are different ways of staging CLL. The older staging systems (namely Rai system and Binet system) are based solely on the volume of CLL in the body as measured by amount of CLL cells in the blood, number of enlarged lymph nodes, spleen, and/or extent of bone marrow involvement.
More important than clinical staging systems like Rai and Binet are the results from more detailed tests like chromosome analysis and gene mutation studies. These tests have been developed only over the last decade and are much better at predicting prognosis and response to treatment than the older clinical staging systems.
Most treatments for CLL do not offer a cure. Treatment is aimed at managing the CLL to the extent that patients can lead a fairly normal life.
In the early stages of CLL, many people will not experience any symptoms and will not need treatment. This is called asymptomatic CLL. Patients will be actively monitored through regular check-ups and blood tests. Treatment will usually begin only when symptoms occur and/or if blood counts drop.
The more common treatment options include small molecule inhibitors (a form of highly targeted therapy), chemotherapy, and biologic (aka monoclonal antibodies) therapy.
Small Molecule Inhibitors (Targeted Therapy)
In CLL, targeted therapy involves using oral drugs (pills) that interfere with specific proteins within the cancer cells to destroy or block their growth. This form of treatment in CLL has come to the forefront in recent years with two such drugs receiving U.S. FDA and Singapore Health Science Authority approval. These drugs are extremely effective and in clinical trials have been shown to be more effective than chemotherapy alone in CLL types that harbour certain genetic mutations.
Chemotherapy
Chemotherapy uses drugs to destroy cancer cells or stop them from multiplying. The drugs may be given intravenously (through a vein in the hand or arm) or in tablet form. Two or more chemotherapy drugs may be combined. Chemotherapy is done in cycles with rest periods in between for the body to recover from the side effects of the drugs. The number of chemotherapy cycles are usually fixed, e.g. 6 – 8 cycles.
Immunotherapy
Immunotherapy involves using monoclonal antibodies, which are man-made immune system proteins, to help the patient’s immune system to identify and destroy cancer cells. The monoclonal antibodies are given intravenously or as injections. Immunotherapy may sometimes be combined with chemotherapy.
Radiation Therapy
In radiation therapy, high-energy X-rays are used to destroy cancer cells in the body. External radiation therapy is provided by a machine outside the body. Radiation therapy is rarely used in CLL.
In 2% to 10% of CLL cases, the leukaemia may transform into an aggressive type of non-Hodgkin lymphoma or to Hodgkin lymphoma. CLL may also progress to prolymphocytic leukeamia. Rarely, CLL may transform into Acute Lymphoblastic Leukaemia (ALL). Certain chemotherapy agents used to treat CLL may also damage the genetic make-up of blood-forming cells in the body.
As there are very few known risk factors for CLL, most of which cannot be avoided, CLL cannot be prevented.

CanHOPE is a non-profit cancer counselling and support service provided by Parkway Cancer Centre, Singapore. CanHOPE consists of an experienced, knowledgeable and caring support team with access to comprehensive information on a wide range of topics in education and guidelines in cancer treatment.
CanHOPE provides:
- Up-to-date cancer information for patients including ways to prevent cancer, symptoms, risks, screening tests, diagnosis, current treatments and research available.
- Referrals to cancer-related services, such as screening and investigational facilities, treatment centres and appropriate specialist consultation.
- Cancer counselling and advice on strategies to manage side effects of treatments, coping with cancer, diet and nutrition.
- Emotional and psychosocial support to people with cancer and those who care for them.
- Support group activities, focusing on knowledge, skills and supportive activities to educate and create awareness for patients and caregivers.
- Resources for rehabilitative and supportive services.
- Palliative care services to improve quality of life of patients with advanced cancer.
The CanHOPE team will journey with patients to provide support and personalised care, as they strive to share a little hope with every person encountered.
