Breast Cancer
Overview
What is breast cancer?
Breast Cancer is a disease in which malignant (cancer) cells are detected in the tissues of the breast. These cells usually arise from the ducts or the lobules in the breast. These cancer cells can then spread within the tissue or organ and to other parts of the body.
Anatomy of the Breast
How common is breast cancer?
Breast cancer is the most commonly occurring cancer in women and the second most common cancer overall. In Singapore, breast cancer is the most common cancer among women. It accounts for close to 30 per cent of the overall frequent cancer incidents in women between 2014 - 2018.* The highest incidence is in the 55 - 59 years age group. The risk of breast cancer increases with age. The good news is that more women are surviving the disease as a result of earlier detection and improved treatment.
*Source: Singapore Cancer Registry Annual Report 2018
Types of breast cancer
There are several types of breast cancer, and they are differentiated by how the cancer cells look under the microscope (called histology); on whether the cancer cells have certain characteristics (receptor status); and on whether they are localised or have spread (stage).
In diagnosing breast cancer, doctors have to distinguish these types of breast cancer carefully so that they can recommend the most appropriate treatment plan for their patients.
Common types of breast cancer
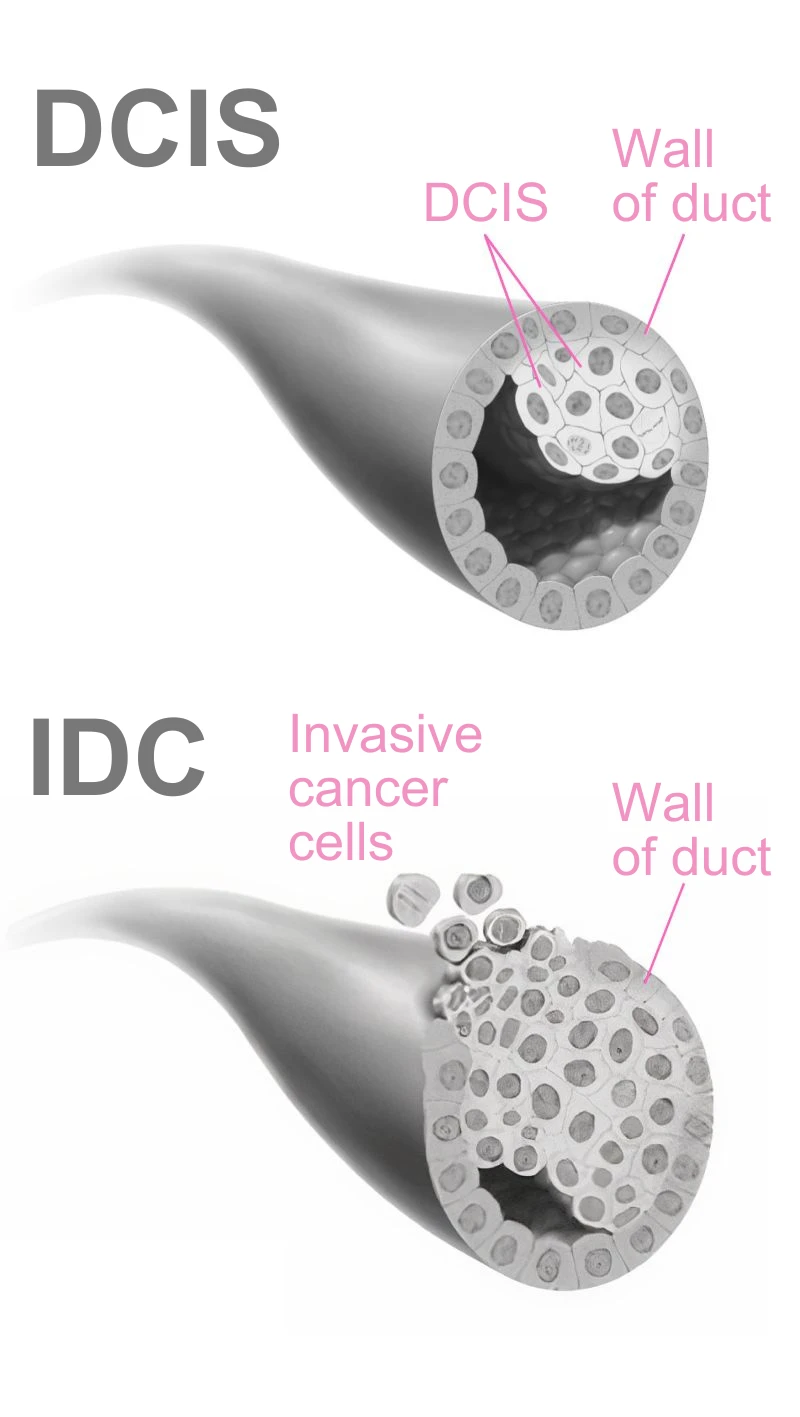
Invasive ductal carcinoma (IDC)
This is the most common type of breast cancer and accounts for 70 to 80 per cent of all cases of invasive breast cancer. The cancer grows in the cells lining the milk ducts in the breast, which then break through the duct wall and invade the breast tissue around the area. These cells may also spread to other organs and parts of the body.
Ductal carcinoma in situ (DCIS)
This is the non-invasive form of IDC, when the cancer does not spread to the surrounding breast tissue. It is also the most common type of non-invasive breast cancer. As it is non-invasive, DCIS is highly treatable, often with surgery alone. It should not be left untreated, however, as it can turn into invasive cancer and spread to other parts of the body.
Invasive lobular carcinoma (ILC)
About 10 per cent of breast cancers diagnosed are of this form of breast cancer, which tends to affect women between 45 and 55 years old. The cancer starts in the cells in the lining of the lobules, the glands that produce milk, and may spread to other parts of the body.
Lobular carcinoma in situ (LCIS)
This non-invasive form of ILC is also known as lobular neoplasia. As LCIS shows no symptoms and cannot be seen with a mammogram, it is usually diagnosed during tests or spotted while treatment is being given for other breast conditions.
Less common types of breast cancer
Medullary carcinoma
Seen in less than 1 per cent of all breast cancer cases, medullary breast cancer tends to hit women who have the inherent faulty BRCA1 gene. The cancer cells are bigger and there is usually a clear demarcation between the tumour and normal tissue.
Tubular carcinoma
Under the microscope, the cancer cells of this form of breast cancer look like tubes. Seen in about 2 per cent of all breast cancer cases, tubular carcinoma tends to affect older women in their 50s and above. It is usually diagnosed through a mammogram.
Inflammatory breast cancer
This aggressive and fast-growing form of breast cancer is seen in 1 to 5 per cent of all breast cancer patients. It can invade the skin and block lymph channels, which can cause redness, swelling and thickening of the overlying skin, and diffuse firmness of the breast.
Mucinous (colloid) carcinoma
Affecting 1 to 3 per cent of breast cancers, this slower-growing cancer tends to affect older women.
Paget disease of the nipple
This cancer, which accounts for 1 to 4 per cent of breast cancers, starts in the breast ducts and spreads to the nipple and the areola – the darker area of the skin around the nipple. It can irritate both and cause them to be scaly, itchy and red.
Breast cancer receptor types
Breast cancers also have different biological characteristics, depending on the presence or absence of receptors such as estrogen receptor (ER), progesterone receptor (PR) and human epidermal growth factor receptor 2 (HER2). These characteristics also affect how the cancer behaves and how it needs to be treated – in some cases, even more than the histology of the cancer.
Hormone receptor-positive breast cancer
Most types of breast cancer (up to 70 per cent) are positive for ER or PR, or both. Such cancers tend to be slower-growing and less aggressive, and patients are, therefore, more likely to have a better long-term outcome. These cancers are usually treated with hormonal therapy such as tamoxifen and aromatase inhibitors.
HER2-positive breast cancer
Some 15 to 25 per cent of women are affected by HER2-positive cancer. This cancer arises when there are excess quantities of the human epidermal growth factor (HER2) protein – found on the surface of normal breast cells – thus causing cells to grow and divide abnormally.
Triple negative breast cancer
This form of cancer does not have ER, PR, or HER2 receptors, and is usually aggressive. The rate of relapse is high, and survival rates are poor. Triple negative breast cancer accounts for about 15 per cent of breast cancers and tend to affect women under 40 and those with a faulty BRCA1 gene.
Causes & Symptoms
Breast cancer risk factors
Studies have shown that the risk of getting breast cancer depends on a combination of factors. Having one or more risk factors does not mean you will get the cancer, but being aware of them can help you to take protective steps to reduce the risk. They include:
- Family history
- Certain inherited genes
- History of malignant or benign (non-cancerous) breast disease
- Early onset of menstruation
- Late menopause
- Having first child after the age of 35
- Having fewer children or never had children
- Being on hormone replacement therapy
- Drinking too much alcohol
- Being overweight or obese
Warning signs of breast cancer
Warning signs of breast cancer include:- Painless lump in the breast
- Persistent itch and rash around the nipple
- Bleeding or unusual discharge from the nipple
- Skin over the breast is swollen and thickened
- Skin over the breast is dimpled or puckered
- Nipple is pulled in or retracted
Diagnosis & Assessment
Diagnosis of breast cancer
Breast cancer can be detected through the following procedures and tests:- Clinical Examination: Especially if a lump, nipple discharge or an unusual breast change is detected.
- Mammogram: This may detect changes such as abnormal densities or calcium deposits.
- Ultrasound Scan: This is used to target a specific area of concern found on the mammogram or may be used to detect abnormalities that are not well seen on the mammogram. An ultrasound scan can distinguish between a solid mass, which may be a cancer, and a fluid-filled cyst, which is usually not cancer.
- Magnetic Resonance Imaging (MRI): In some cases, patients go for a MRI scan to better screen or examine suspicious areas. This is particularly useful for younger women because younger women have an increased breast tissue density and conventional imaging tests such as mammogram or ultrasound are less sensitive and specific for detecting breast cancer.
To confirm breast cancer, a biopsy will have to be performed in which cells or a piece of tissue is removed for examination under a microscope.
Common biopsy techniques:
- Fine Needle Aspiration (FNA)
- Core Needle or Tru-cut Biopsy
- Excision Biopsy
How is breast cancer assessed?
If the biopsy shows that cancer is present, your doctor needs to know the extent of the disease to plan the best treatment. Staging of breast cancer is based on whether the tumour has invaded nearby tissues, whether the cancer has spread and, if so, to what parts of the body.Stages / Extent of Spread
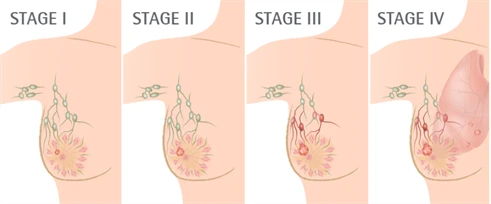
| Stages | Extent of Spread | Average 5-Year Survival Rate (%) | |
| 0 | Non invasive cancer | 99 | |
| I | Small invasive cancer | 90 | |
| II | Invasive cancer | 70 | |
| III | Large invasive cancer | 40 | |
| IV | Widespread or metastatic cancer | 20 |
Characteristics of breast cancer that impacts on relapse and survival
Tumour Size
In general, the larger the size of tumour the greater the chance of breast cancer reoccurring.
Tumour Grade
Histologic Grade: This refers to how much the tumour cells resemble normal cells when viewed under the microscope; the grading scale is 1 to 3. Grade 3 tumours contain rapidly growing cancer cells. The higher the histologic grade, the greater the chance of breast cancer relapsing.
Lymph Nodes
The number of lymph nodes that is in the armpit, on the same side of the affected breast, is an important indicator. A higher number of positive nodes is associated with a worse outcome and warrants more aggressive treatments.
ER/PR
About two-thirds of all breast cancers contain significant levels of estrogen and/or progesterone receptors. They are referred to as estrogen receptor positive (ER+) tumours. ER-positive tumours tend to grow less aggressively and may respond favorably to treatment with hormones.
HER2/erbB2
HER2 is a protein found on the surface of certain cancer cells. A tumour is described as being HER2-positive when it has a lot more HER2 receptors than others. About 20-25% of all breast cancers have tumours labelled HER2- positive. Tumours that are HER2-positive tend to grow more quickly than other types of breast cancer. By knowing if a cancer is HER2-positive can affect the choice of treatment because women with such tumour can benefit from anti Her2 targeted therapy.
Treatment
Treatment options and prognosis (chance of recovery) depends on the stage of the cancer (whether it is in the breast only or has spread to other places in the body), the type of breast cancer, certain characteristics of the cancer cells and whether the cancer is found in the other breast. A woman’s age, menopausal status (whether a woman still has menstrual periods) and her general health can also affect treatment options and prognosis.
Surgery
Most have surgery to remove the cancer. Forms of surgery include:
1. Breast – conserving surgery
- Lumpectomy or Wide Local Excision – removal of the cancer and a small amount of surrounding tissue
- Quadrantectomy – removal of more surrounding tissue than a lumpectomy. For a quadrantectomy, one-quarter of the breast is removed.
2. Mastectomy – removal of the whole breast.
During both of the above breast surgeries, some of the lymph nodes under the same armpit will also be removed for examination.
Systemic Therapy
- Chemotherapy
- Anti Cancer Hormone Therapy
- Targeted Chemotherapy
Radiotherapy
Radiotherapy uses high-energy rays to target and kill cancer cells. The goal is to kill any cancer that might be left in or around the breast.
Radiotherapy is vital after a breast-conserving surgery like lumpectomy, since much of the breast tissue is left intact. It will lower the chances of the cancer returning in the breast.
Most women who have a mastectomy do not need radiotherapy. However, in some cases, it is used to treat the chest wall and the lymph nodes in the armpit, if the risk of local recurrence is determined to be high enough based on size and margin.
Rehabilitation
Physical rehabilitation includes:
- Shoulder exercises after surgery
- Arm care to avoid lymphoedema
- Balanced nutrition and lifestyle adaptation to enhance recovery
Mental rehabilitation involves:
- Close support of spouse, family, friends and support groups
- A woman may feel reassured by knowing her chances of survival
- Attending doctor reviews regularly
Prevention & Screening
Breast cancer screening
Screening usually involves checking your breasts for cancer even before there are any signs and symptoms. While screening cannot prevent breast cancer, it can help you to detect the cancer early, so that it can be treated earlier.
In general, screening tests include:
- Mammogram
- Ultrasound scan
- Breast MRI
- Breast self-examination (BSE)
Breast Cancer Screening Guideline
39 years and below |
|
40 to 49 years |
|
50 years and above |
|
Frequently Asked Questions (FAQ)
You can reduce your risk through lifestyle choices such as maintaining a healthy weight by having a balanced diet, exercising regularly, limiting your intake of alcohol, and not smoking (or quitting if you smoke).
Read more at Breast Cancer Screening: Why bother?
You can take steps to monitor your breasts so as to be aware of any anomalies and changes through physical signs, screening tests and perform breast self-examinations.
Breast cancer may return despite the best care and treatment. When this happens, it is called a recurrence or relapse. A relapse may occur when some of the original cancer cells survive the initial treatment, or when cancer cells spread to other parts of the body while being undetected.
Some of the more common risk factors that may affect the chances of breast cancer returning include:
- Tumour size – Large tumours usually point towards a greater chance of cancer recurrence.
- Cancer spread – Breast cancer is more likely to recur if it had spread to the lymph nodes.
- Cancer subtypes – Some breast cancer subtypes like HER2-positive breast cancer are more likely to recur.
