Hyperthermia
.webp?sfvrsn=a3cedba7_1)
Overview
What is hyperthermia?
Hyperthermia is a cancer treatment that uses heat to destroy cancer cells and shrink tumours.[1] The treatment works by raising the temperature of cancer tissue to between 39°C and 45°C for approximately one hour.[1,9] When cells in the body are exposed to higher-than-normal temperatures, they undergo changes that can make them more susceptible to other cancer treatments, such as radiation therapy or chemotherapy.[1] In some cases, the heat itself can directly kill cancer cells, though hyperthermia is almost always used in combination with other forms of cancer treatment rather than as a standalone therapy.[3]
How does hyperthermia work?
Hyperthermia enhances the effectiveness of other cancer treatments through several mechanisms.[2] The heat increases blood flow to the tumour area, which allows more oxygen and medications to reach the cancer cells.[1,9] This increased oxygen delivery makes tumour cells more sensitive to radiation therapy, as oxygen is essential for radiation to damage and kill cancer cells.[3] Additionally, heat interferes with the ability of cancer cells to repair damage caused during radiation therapy, particularly disrupting DNA repair mechanisms.[1,9] When combined with chemotherapy, hyperthermia can enhance the delivery of anticancer drugs to the tumour area and improve their effectiveness.[2] Hyperthermia can also stimulate the immune system in some patients, potentially helping the body's natural defences fight cancer.[4,9]
Unlike normal cells, which can better tolerate heat due to efficient blood circulation, cancer cells are already stressed by low oxygen levels, higher acid concentrations, and insufficient nutrients within the tumour environment.[7] This makes them less able to withstand the effects of elevated temperatures, giving hyperthermia a therapeutic advantage.[7,9]
Conditions suitable for hyperthermia
Hyperthermia therapy can be particularly beneficial for several types of cancers and certain treatment-resistant or recurrent tumours.[9] Conditions that may benefit include:
Superficial tumours: Cancers close to the skin's surface, such as melanoma, recurrent breast cancer, and head and neck cancers, respond well to hyperthermia because these tumours are easily accessible for localised heat application.[9]
Deep-seated tumours: Hyperthermia can also target deeper tumours when combined with other treatments. Cancers of the cervix, bladder, rectum, and prostate can benefit, especially when hyperthermia is used with radiotherapy to enhance treatment effects.[9]
Recurrent tumours: Hyperthermia is often effective in cases where cancer recurs in a previously treated area. Radiation doses are limited in repeat treatments due to the risk of damaging surrounding healthy tissue, but adding hyperthermia can help overcome this challenge by enhancing the effects of radiation at lower doses.[9]
Tumours with hypoxic or resistant cells: Cancers with low-oxygen cells are typically more resistant to radiation. Hyperthermia improves blood flow and oxygenation in the tumour, making these cells more sensitive to radiation.[9]
Soft tissue sarcomas: Hyperthermia has shown success in treating certain soft tissue sarcomas, especially when combined with radiation or chemotherapy.[1,9]
Advanced or unresectable tumours: In cases where tumours are inoperable due to size, location, or stage, hyperthermia can help to control tumour growth, reduce symptoms, and potentially improve overall treatment outcomes when used as an adjunct therapy.[9]
Who is suitable to receive hyperthermia?
Hyperthermia is not widely available yet, but at specialised cancer centres, it is used for select patients with advanced cancers.[2] Your doctor will evaluate and recommend whether hyperthermia is suitable for your specific situation after reviewing your medical history, cancer type, and overall health status.
However, certain individuals may not be suitable candidates for hyperthermia:[9]
- Patients whose treatment area has metal implants (such as joint replacements or pacemakers) that can absorb heat and make temperature control difficult
- Those with serious cardiovascular or respiratory conditions who may have difficulty tolerating the increased body temperature and blood flow
- Pregnant individuals, due to potential risks to the foetus
- Patients with certain autoimmune diseases that may make them more susceptible to tissue damage
- Those with compromised skin integrity or extensive skin wounds
- Patients who are unable to tolerate elevated temperatures due to individual sensitivity
Receiving Hyperthermia
Types of hyperthermia
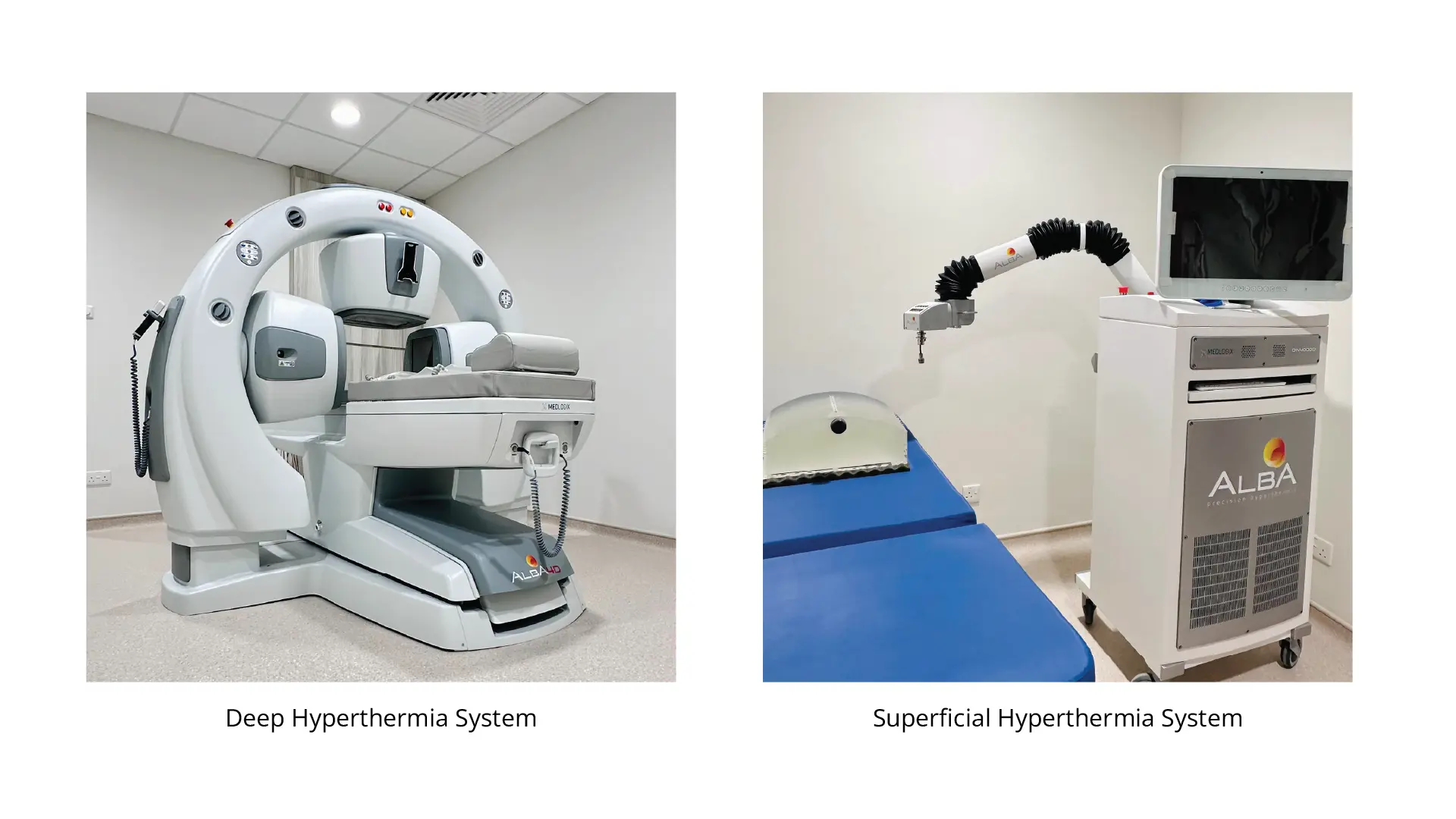
There are two types of hyperthermia treatments offered at our facilities: superfacial hyperthermia and deep hyperthermia.
Superficial hyperthermia is used to treat tumours near the skin by applying external devices directly on the surface, using microwave / radiofrequency energy specifically set to heat only shallow tissues.[9] Deep hyperthermia targets tumours located deeper than 4cm beyond the skin in the body, such as those in the pelvis or abdomen.[9]
Before your hyperthermia treatment
Before undergoing hyperthermia, your healthcare team will:[1,5,9]
- Perform imaging exams such as CT scans to pinpoint the exact location requiring treatment
- Order blood tests to ensure you are healthy enough for the procedure
- Evaluate possibility of not suitable to receive hyperthermia
- Provide instructions about eating or drinking before treatment
- Advise you to stop taking certain medications, particularly blood thinners
On the day of treatment, a nurse or radiation therapist will explain the procedure to you, including how long it will take and what you need to do.[9] You will be positioned on the treatment couch in the same way as during your simulation to ensure the setup is exactly right.[9] A nurse will check and record your vital signs (such as blood pressure and heart rate) to make sure you're stable before starting.[9]
For superficial hyperthermia, a special transparent template will be placed on the treatment area to help guide the placement of temperature sensors.[9] For deep hyperthermia, a catheter may be inserted in the body with sensors placed inside it for internal temperature monitoring.[9]
During your hyperthermia treatment
The specific method of administering hyperthermia depends on the type and location of the cancer.[2] During treatment, your doctor will use specialised thermometers and temperature probes to monitor your body temperature continuously, ensuring the heat is delivered safely and effectively.[1,9] Imaging techniques, such as ultrasound, MRI, or CT scans, may be used to guide probe placement and ensure accuracy.[3]
Treatment sessions usually last between 60 and 90 minutes, depending on the treatment plan.[9] Once the pre-treatment setup is complete, the therapist will ask you to remain still and to let them know if you experience any pain during the process.[9] A radiation oncologist will review the setup and treatment parameters before the treatment begins.[9]
During hyperthermia treatment, you can expect the following experiences and effects:[9]
- Sensation of warmth: The targeted area will typically feel warm during the procedure. The intensity of this warmth depends on factors such as how deep the tumour is located, which part of the body is being treated, and how long the session lasts.
- Possible mild discomfort: Some patients experience slight discomfort where heat is being applied. For tumours near the skin surface, you might notice your skin feels warm or appears flushed. When treating deeper tumours, patients sometimes describe sensations of internal warmth or pressure.
- Body positioning and support: The treatment team will position you using pillows and other supportive devices to keep you comfortable throughout the session. Depending on which area requires treatment, certain hyperthermia equipment may necessitate a particular body position.
- Monitoring by the medical team: The radiation therapist will track your response throughout the procedure, making necessary adjustments to achieve the target temperature and therapeutic goals. A nurse will reassess your vital signs approximately halfway through the treatment, documenting all modifications and observations in the treatment record.
- Potential skin reactions: Following treatment, especially with superficial hyperthermia, the application site may develop mild redness, feel tender, or appear slightly swollen. These reactions are typically short-lived and resolve soon after treatment concludes.
- Communication with the care team: You can speak with your healthcare team at any point during the session. This ensures your comfort is maintained and allows any concerns or uncomfortable sensations to be addressed immediately.
After your hyperthermia treatment
Once the treatment is finished, a nurse will take and record your vital sign parameters.[9] The antenna and the template (with the attached sensors) are carefully removed from your body.[9] A radiation therapist will help you off the treatment couch and accompany you out of the room.[9] If there is a review appointment on the same day, you will meet with the radiation oncologist; if not, you will be reminded of your next scheduled appointment.[9] Do pay attention to the instructions about your radiotherapy appointment time, which could be before or after the hyperthermia treatment on the day it is scheduled. Typically, hyperthermia is prescribed once or twice per week, while radiotherapy is prescribed as a daily treatment (Monday to Friday).
In most cases, hyperthermia is an outpatient procedure, meaning you can go home the same day.[4] You may feel a bit tired after hyperthermia treatment, as the body expends energy in response to the heat. This fatigue is usually mild and improves with rest.[9] The treatment room may be kept at a comfortable temperature, and you are encouraged to stay hydrated before and after treatment to prevent dehydration.[9]
Risks and Complications
What are the risks and complications of hyperthermia?
Hyperthermia therapy, whilst generally well-tolerated, does carry some risks and potential complications.[9] These can vary based on the treatment area, temperature, and your overall health. The side effects of hyperthermia are generally minimal, especially compared to chemotherapy or radiation therapy alone.[2]
Potential risks and complications may include:[1,3,9]
- Skin burns: Overheating the skin or tissues near the treatment area can cause burns, especially in superficial hyperthermia where heat is applied closer to the skin.
- Pain or discomfort: Some patients may feel mild to moderate pain or discomfort in the treated area, particularly if the temperature is difficult to control or maintain evenly. This can include a sensation of warmth or even mild tenderness after treatment.
- Fatigue and malaise: General tiredness or feeling unwell is a possible side effect due to the body's reaction to the heat, especially in whole-body hyperthermia treatments.
- Local sensitivity and pigmentation changes: Some patients may experience sensitivity in the treated area or temporary skin colour changes. These changes are usually temporary but can sometimes last for several weeks post-treatment.
Most side effects improve shortly after treatment ends.[1] Serious side effects are uncommon, though some patients may experience cardiovascular effects.[4] Close monitoring and precise temperature control are key to minimising these risks.[9] Hyperthermia treatments are often adapted to each patient's tolerance, with lower temperatures used if needed to reduce side effects.[9]
Your healthcare team will monitor you closely during and after treatment to manage any side effects that occur. Your doctor will be able to discuss detailed specific side effects relevant to your condition.[9]
Is hyperthermia safe?
Hyperthermia is considered a safe treatment when administered by experienced specialists at qualified cancer centres.[3] The key to safety is precise temperature monitoring and control to ensure the heat damages cancer cells whilst minimising harm to surrounding healthy tissue.[1] Because temperature management is critical for both safety and effectiveness, hyperthermia should only be performed by doctors with specialised training in this technique.[2]
Recovery and Outlook
Recovery after hyperthermia
Recovery depends on the type of hyperthermia you received.[3] For outpatient procedures, most patients can resume their usual activities within a few days.[1] Your doctor may prescribe pain medication to manage any discomfort during the recovery period.[4]
Your doctor will monitor your progress through periodic blood tests and imaging exams to determine whether the treatment has reduced tumour size or eliminated cancer cells.[1] Follow-up appointments are an important part of your care plan, as they help your medical team assess treatment effectiveness and make any necessary adjustments to your overall cancer treatment strategy.[2]
Effectiveness
Research has shown that hyperthermia, when used in combination with radiation therapy or chemotherapy, can improve treatment outcomes.[6,8] Clinical studies demonstrate that hyperthermia can significantly increase treatment response rates without adding toxicity when carefully applied, as it affects tumour cells more than surrounding healthy tissues.[9] Hyperthermia can help shrink tumours, enhance the effectiveness of other cancer treatments, and may improve survival rates for select cancer types.[6] However, hyperthermia is still considered an emerging treatment at many centres.[7] Research is ongoing, and the use of hyperthermia in combination with immunotherapy and other advanced treatments is showing promise in expanding its potential applications.[9] Your doctor will discuss what outcomes you can realistically expect based on your specific cancer type and treatment plan.
