Liver Cancer
Overview
What is Liver Cancer?

Liver cancer refers to the growth of abnormal cells in the liver.
How Common is Liver Cancer?
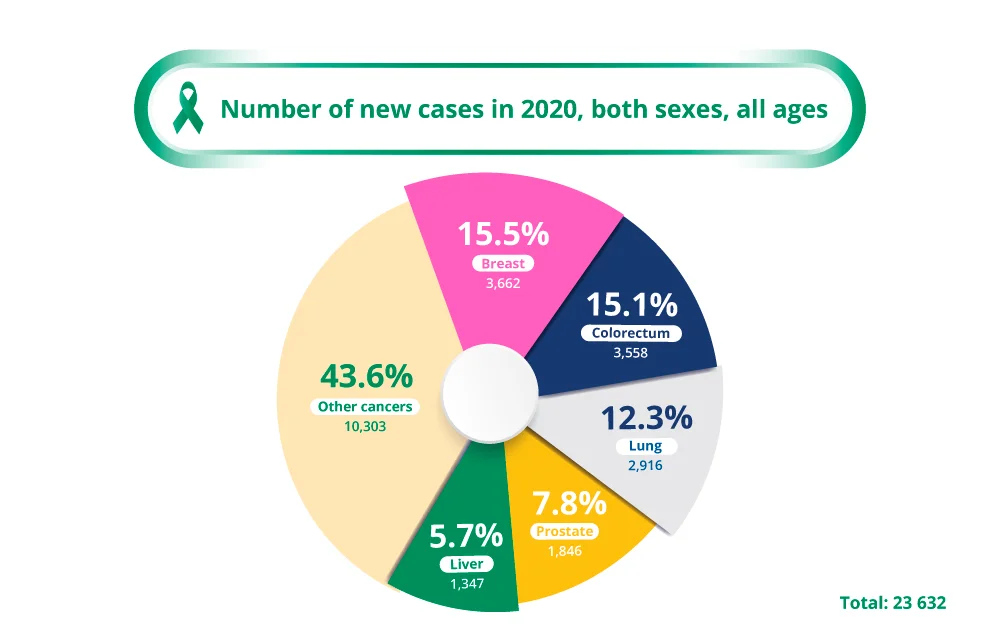
Primary liver cancer is the fifth most common cancer in Singapore, accounting for 5.7% of all new cancers diagnosed in the whole population3. It is more common in Asian countries mainly due to high levels of chronic viral hepatitis in the community, which is a major risk factor for liver cancer. Nearly three quarters of the world’s population of chronic hepatitis B carriers live in Asia4.
The good news is that liver cancer cases in Singapore have been declining steadily over recent years. This favourable trend is largely attributed to the implementation of the hepatitis B childhood vaccination programme since 1985, as well as the advent of effective anti-viral medication to treat chronic hepatitis C infection5.
Types of Liver Cancers
Liver cancer can be classed as primary or secondary, based on where the cancer cells originated from1.
Primary liver cancer occurs when the cancer arises from the cells in the liver itself. The different types of primary liver cancer are usually named after the types of cells from which the cancer has developed from. Hepatocellular carcinoma (HCC) or hepatoma arises from the main cells of the liver called hepatocytes and accounts for more than 80% of primary liver cancers2. A less common type of primary liver cancer originates from cells that line the bile duct called cholangiocytes and is therefore called cholangiocarcinoma or bile duct cancer.
Secondary (or metastatic) liver cancer occurs when the main cancer originates elsewhere in the body and deposits cancer cells in the liver. This type of cancer is named after the organ that it originated from. A common example of this is metastatic colorectal cancer, which is cancer of the colon or rectum that spreads to the liver via the bloodstream.
In the rest of this content, liver cancer refers to primary hepatocellular carcinoma.
Causes & Symptoms
What causes Liver Cancer?
Liver cancer occurs when cells in the liver develop mutations (changes) in their DNA which lead to abnormal growth and the formation of a cancerous tumour. Sometimes the cause is known, such as in chronic hepatitis infections. However, at times, liver cancer can form without underlying disease and no clear cause for it.6
Liver Cancer Risk Factors
Doctors may not always have an explanation as to why one person develops liver cancer, and another does not. However, there are certain risk factors that increase the likelihood of a person developing liver cancer, including7:
Chronic viral hepatitis
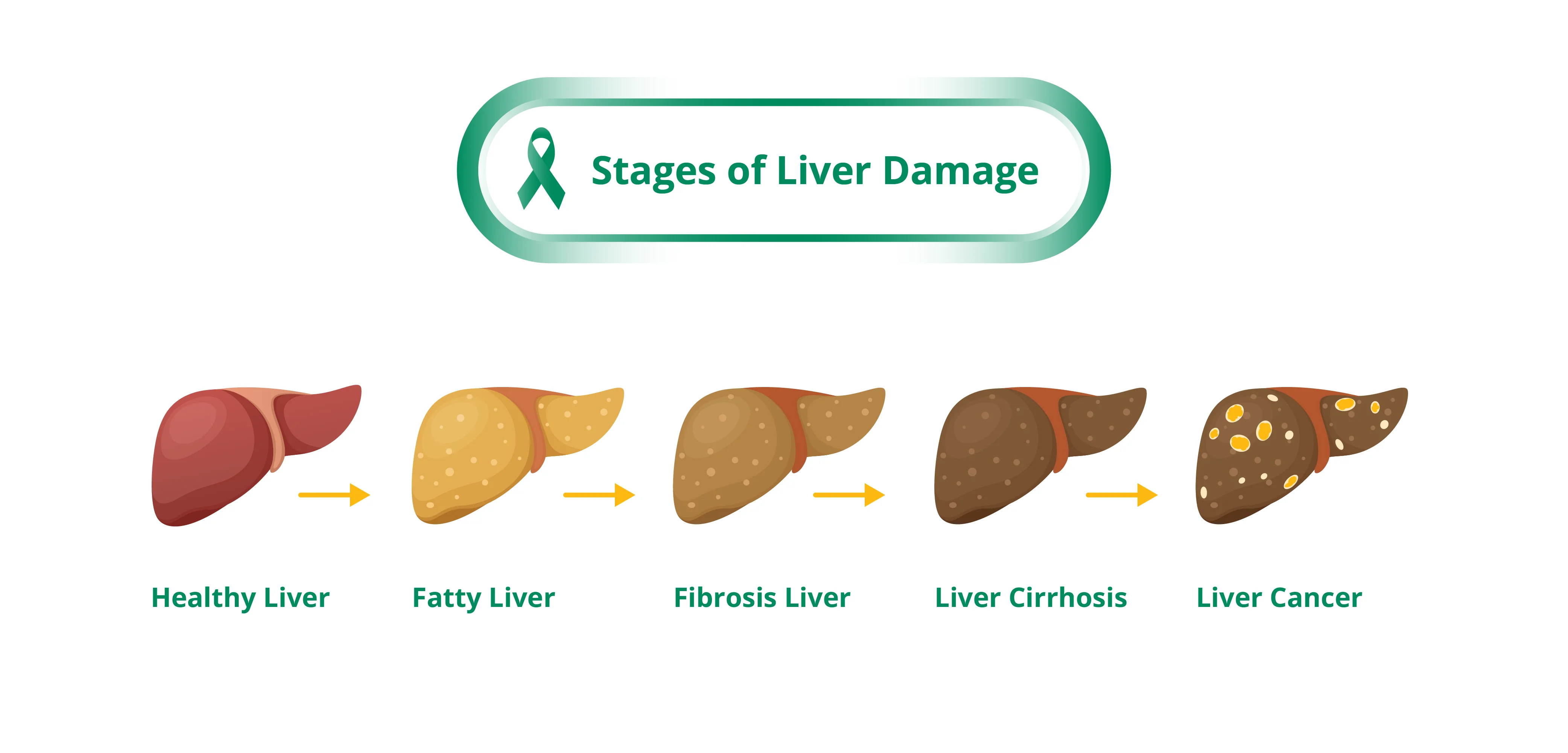
Chronic hepatitis B and C virus infections account for 80% of hepatocellular cancer (the most common primary liver cancer) globally2.Alcoholic cirrhosis
Heavy alcohol intake over many years can lead to cirrhosis (irreversible scarring of the liver) which can then progress to liver cancer.Non-alcoholic fatty liver disease (NAFLD)
This condition, where there is accumulation of fat in the liver, is becoming a growing problem in Asia due to increasingly inactive lifestyle and dietary factors leading to obesity4.Type 2 Diabetes
Type 2 Diabetes has been linked with an increased risk of liver cancer, particularly in those with chronic viral hepatitis and heavy alcohol intake.Exposure to aflatoxins
Aflatoxins are cancer-causing substances made by a fungus that contaminates peanuts, wheat, soybeans, ground nuts, corn, and rice which have been stored in a warm, moist environment.Inherited metabolic diseases
These include hemochromatosis (a disorder in which there is too much iron in the body) and Wilson's disease (a disorder in which excess copper builds up in the body).
Many liver cancers can be prevented by public health measures that reduce exposure to these known risk factors.
What are the Signs and Symptoms of Liver Cancer?
The early stages of liver cancer often do not cause symptoms. The first signs and symptoms of liver cancer are quite non-specific as most of them can also be attributable to other health conditions6:
- Loss of weight without trying
- Loss of appetite
- Feeling full after a small meal
- Upper abdominal (belly) pain
- Nausea and vomiting
- General weakness and fatigue
In more advanced stages, the following signs of liver failure may be present8:
- Jaundice (yellow discoloration of your skin and the whites of your eyes)
- White, chalky stools
- Dark urine
- Abdominal swelling from fluid build-up
- Bleeding from the gut
- Abnormal bruising
- Altered mental state
Diagnosis & Assessment
Diagnosis of Liver Cancer
The following tests and procedures may be performed to diagnose liver cancer9:
Physical examination
An examination of the abdomen is performed to check for hard masses, ascites (fluid in the abdomen) and other signs of liver disease.Blood tests
To check liver function and alpha-fetoprotein (AFP) levels. AFP is a tumour marker in the blood that can be higher in people with liver cancer.Liver ultrasound
A scan that uses sound waves to produce a picture of the liver. This is a painless test and usually takes several minutes to perform. The picture may reveal a liver tumour.Computed tomography (CT) or magnetic resonance imaging (MRI)
Scan of the abdomen to visualise the three-dimensional picture of the liver and surrounding organs. It can show the size and position of a tumour, blood vessels and whether the cancer has spread elsewhere.Liver biopsy
A small sample of tissue is removed via a biopsy needle and examined under a microscope. It is not usually necessary or advised in liver cancer cases as it carries a potential risk of bleeding and spreading the tumour.
How is Liver Cancer Assessed?
After liver cancer has been diagnosed, your doctor will determine the extent (stage) of the disease. Staging, usually done with CT scans, PET-CT scans or MRI, is done to find out whether the cancer has spread, and if so, to what parts of the body. Liver cancer spreads most often to the lymph nodes, lungs and bones. The stages of liver cancer are10:
Stage 1
The single primary tumour has not grown into any blood vessels or spread to nearby lymph nodes nor distant sites.Stage 2
A single primary tumour has grown into blood vessels in the liver, or several smaller tumours are present, but the cancer has not spread to nearby lymph nodes nor distant sites.Stage 3
Several tumours with at least one large tumour, or at least one has grown into blood vessels in the liver, but the cancer has not spread to nearby lymph nodes nor distant sites.Stage 4
The cancer has spread to nearby lymph nodes and/or to distant sites in the body.
Staging of liver cancer is not as straightforward as for other cancers. Apart from tumour characteristics and degree of spread, the outcome for liver cancer also depends on the degree of liver impairment, as there is often damage to the liver that affects its function10. For example, someone diagnosed with stage 4 liver cancer and normal liver function will likely outlive someone else with stage 2 liver cancer who is in end stage liver failure.
Treatment of Liver Cancer
Liver Cancer Treatment Options
The type of treatment for patients with liver cancer will depend on its stage (that is, its size and whether it has spread beyond its original site), the patient’s general health and liver function. The main treatments used are surgery, tumour ablation, chemotherapy, targeted cancer therapy and radiotherapy11:
Surgery
Surgery is potentially curative and is therefore the treatment of choice for patients with early-stage liver cancer2. If only certain parts of the liver are affected by cancer and the rest of the liver is healthy, then surgery may be possible to remove the affected part(s). This type of surgery is called a liver resection (partial hepatectomy).
Another form of surgery is a liver transplantation. This involves the removal of the entire liver and replacement with a healthy donated liver. Such a major operation may be performed when the cancer is in the liver only and a donated liver is available.
If surgery is not possible, then other treatments may be offered to help control the cancer, thereby reducing symptoms and improving quality of life.Tumour ablation
Tumour ablation aims to destroy primary liver cancer cells using either heat (radiofrequency ablation; RFA) or alcohol (percutaneous ethanol injection; PEI). This procedure is usually done in the scanning department so that ultrasound or computerised tomography (CT) can help the doctor to guide a needle through the skin and into the cancer within the liver. A local anaesthetic will be given.
RFA treatment uses laser light or radio waves passed through the needle to destroy cancer cells by heating them to a very high temperature. PEI treatment uses alcohol injected through the needle into the cancer to destroy the cancer cells. Tumour ablation may sometimes be repeated if the tumour grows again.Chemotherapy
Chemotherapy is the use of anti-cancer drugs to destroy cancer cells or stop them from dividing. It can help to control symptoms by shrinking the cancer and slowing its progression. Chemotherapy drugs are usually given as injections into the vein (intravenously), although they can sometimes be given as tablets. Chemotherapy may also be administered as part of a treatment called chemoembolisation.
Chemoembolisation involves the injection of chemotherapy drugs directly into the cancer in the liver, together with a gel or tiny plastic beads to block blood flow to the cancer (embolisation). Not everyone is suitable for chemotherapy as it can only be given if the liver function is good enough.Targeted drug therapy
Targeted drug therapy uses drugs or other substances that block the growth and spread of cancer by interfering with specific molecules involved in cancer growth and progression.
There are a few targeted drugs available to treat liver cancer. These drugs target cancers by stopping them from growing their own blood vessels. As cancer cells need a blood supply to bring nutrients and oxygen, this drug may therefore limit the cancer’s ability to develop. These drugs have been demonstrated in large clinical studies to prolong survival in patients with advanced liver cancer, compared to supportive care alone2,12.Immunotherapy
An important part of the immune system is the ability to recognise foreign from normal cells.
Immunotherapy is a relatively new form of therapy where patients receive a medication targeted at a receptor called the programmed death protein 1 (PD1) or programmed death ligand 1 (PD- L1). These are known as checkpoint inhibitors. These drugs stimulate the immune cells called T lymphocytes to attack the cancer cells. A number of immunotherapy drugs have been shown to be useful in liver cancer and more clinical trials are underway2,12.Radiotherapy
Radiotherapy uses high-energy rays to destroy cancer cells or keep them from growing. External radiotherapy uses a machine outside the body that delivers radiation towards the cancer. Such treatment is not often used to treat liver cancer because the liver cannot take very high doses of radiation. It may however be used to relieve pain, for example, in patients whose cancer has spread to the bone.
Alternatively, internal radiation uses a radioactive substance delivered selectively to the cancer via a major blood vessel that carries blood to the liver (hepatic artery).
Liver Cancer Survival Rate
Early diagnosis of liver cancer increases the likelihood for cure2.
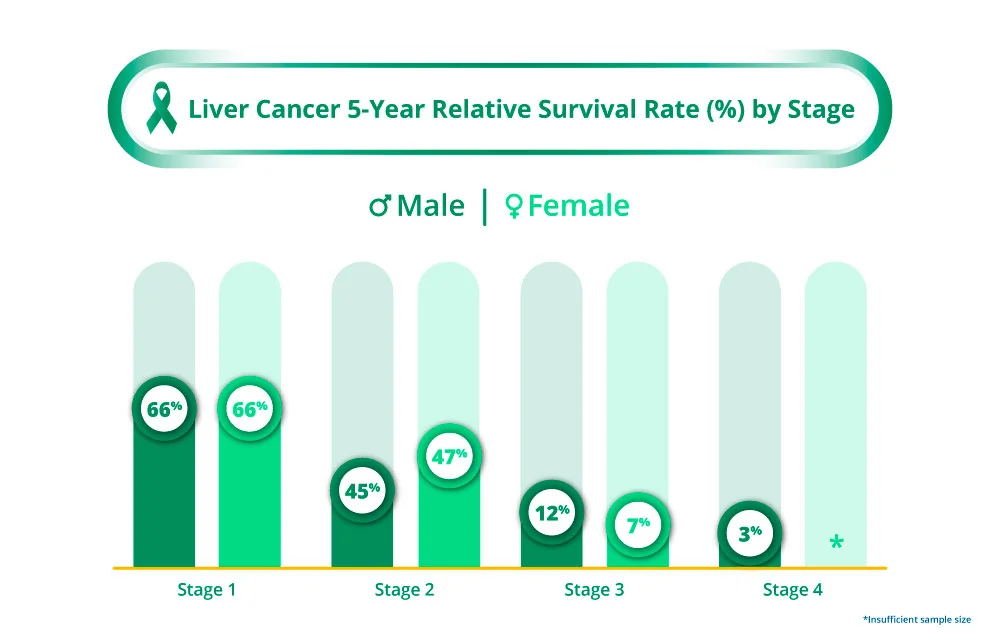
It is important to bear in mind that these rates are estimates and with continued advancements in treatment as well as screening methods, the life expectancy with liver cancer is expected to continue to improve.
Prevention & Screening
Liver Cancer Screening
Screening refers to looking for cancer before a person has any symptoms. Screening can help doctors find and treat liver cancer early, when the cancer is localised and more easily removed by surgery. This may in turn improve the chance of survival13. For the general population, screening for liver cancer has not been shown to reduce the chances of dying from liver cancer and is not generally recommended6.
People with increased risk of getting liver cancer, such as those with chronic hepatitis B infection and liver scarring (cirrhosis) due to hepatitis C or other causes, should be screened for liver cancer. Screening involves:
- A blood test for alpha-fetoprotein (AFP) every 3-6 months
- An ultrasound scan of the liver every 6-12 months
Liver Cancer Prevention
While there is no guaranteed way to prevent liver cancer, there are some measures you can take to reduce your risk4:
- Vaccinate against hepatitis B virus
- Seek treatment for hepatitis B and C infections
- Maintain a well-balanced, healthy diet such as the Mediterranean diet
- Drink alcohol in moderation, if at all
- Avoid dietary aflatoxin exposure by not eating mouldy or improperly stored corn, rice, wheat, peanuts and soybeans products
- Stay active with regular exercise and maintain a healthy body weight
- Go for regular screening if you are in the high-risk group
Frequently Asked Questions (FAQ)
It is often difficult to detect liver cancer early because signs and symptoms usually do not appear until it has progressed to the later stages of the disease. There is currently no recommended screening tests for the general population6.
If you are at high risk for liver cancer, for example, if you have chronic hepatitis B infection and liver scarring (cirrhosis) due to hepatitis C or other causes, 6-monthly surveillance with a blood test for alpha-fetoprotein (AFP) and an ultrasound scan of the liver will increase the chances of early detection should you develop liver cancer.
Liver cancer may be curable if diagnosed at an early stage when the cancer has not spread. In these cases, surgical resection (removal of the whole tumour), or liver transplantation is the best option for cure. Small liver cancers may also be cured with other types of treatment such as ablation or radiation.14
The liver is a vital organ that filters waste products in the blood, eliminates toxins, breaks down and stores nutrients, and produces substances that help blood clot. You cannot survive without a liver, but you can live with part of a liver or a liver that is not functioning properly.
The liver is the only solid organ in the human body that can regenerate itself. In fact, it is possible for the liver to regrow even when up to 90% of the liver is absent15. For this reason, if a person needs a liver transplant, a living donor only needs to donate part of their liver. The remaining parts of the liver then regrow in both the donor and the recipient.
This self-regeneration process, however, can be damaged following persistent insults to the liver, as in the case with chronic liver diseases.
References
- American Cancer Society. What is Liver Cancer? Accessed at https://www.cancer.org/cancer/types/liver-cancer/about/what-is-liver-cancer.html on 17 July 2023.
- Yang JD. et al. A Global View of Hepatocellular Carcinoma: Trends, Risk, Prevention and Management. Nature Reviews Gastroenterology & Hepatology. 2019 Oct; 16(10): 589–604.
- The Global Cancer Observatory, International Agency for Research on Cancer, World Health Organization. Singapore Fact Sheet. Accessed at https://gco.iarc.fr/today/data/factsheets/populations/702-singapore-fact-sheets.pdf on 17 July 2023.
- Jafri W. et al. Hepatocellular Carcinoma in Asia: A Challenging Situation. Euroasian Journal of Hepatogastroenterology. 2019 Jan-Jun; 9(1): 27–33.
- Liu Y. et al. Changes in the Epidemiology of Hepatocellular Carcinoma in Asia. Cancers. 2022 Sep; 14(18): 4473.
- Mayo Clinic. Liver Cancer Symptoms and Causes. Accessed at https://www.mayoclinic.org/diseases-conditions/liver-cancer/symptoms-causes/syc-20353659 on 17 July 2023.
- American Cancer Society. Liver Cancer Risk Factors. Accessed at https://www.cancer.org/cancer/types/liver-cancer/causes-risks-prevention/risk-factors.html on 17 July 2023.
- American Cancer Society. Signs and Symptoms of Liver Cancer. Accessed at https://www.cancer.org/cancer/types/liver-cancer/detection-diagnosis-staging/signs-symptoms.html on 17 July 2023.
- Gleneagles Hospital Singapore. Liver Cancer Diagnosis and Treatment. Accessed at https://www.gleneagles.com.sg/conditions-diseases/liver-cancer/diagnosis-treatment on 17 July 2023.
- Cancer Research UK. About staging of liver cancer. Accessed at https://www.cancerresearchuk.org/about-cancer/liver-cancer/stages/about-staging-of-liver-cancer on 17 July 2023.
- Mayo Clinic. Liver Cancer Diagnosis. Accessed at https://www.mayoclinic.org/diseases-conditions/liver-cancer/diagnosis-treatment/drc-20353664 on 17 July 2023.
- UpToDate. Systemic treatment for advanced hepatocellular carcinoma. Accessed at https://www.uptodate.com/contents/systemic-treatment-for-advanced-hepatocellular-carcinoma on 17 July 2023.
- National Registry of Diseases Office. Singapore Cancer Registry 50th Anniversary Monograph – Appendices. Singapore, National Registry of Diseases Office; 2022.
- American Cancer Society. Surgery for Liver Cancer. Accessed at https://www.cancer.org/cancer/types/liver-cancer/treating/surgery.html on 17 July 2023.
- National Institutes of Health. Cells that maintain and repair the liver identified. Accessed at https://www.nih.gov/news-events/nih-research-matters/cells-maintain-repair-liver-identified on 17 July 2023.
