Myelodysplastic Syndromes (MDS)

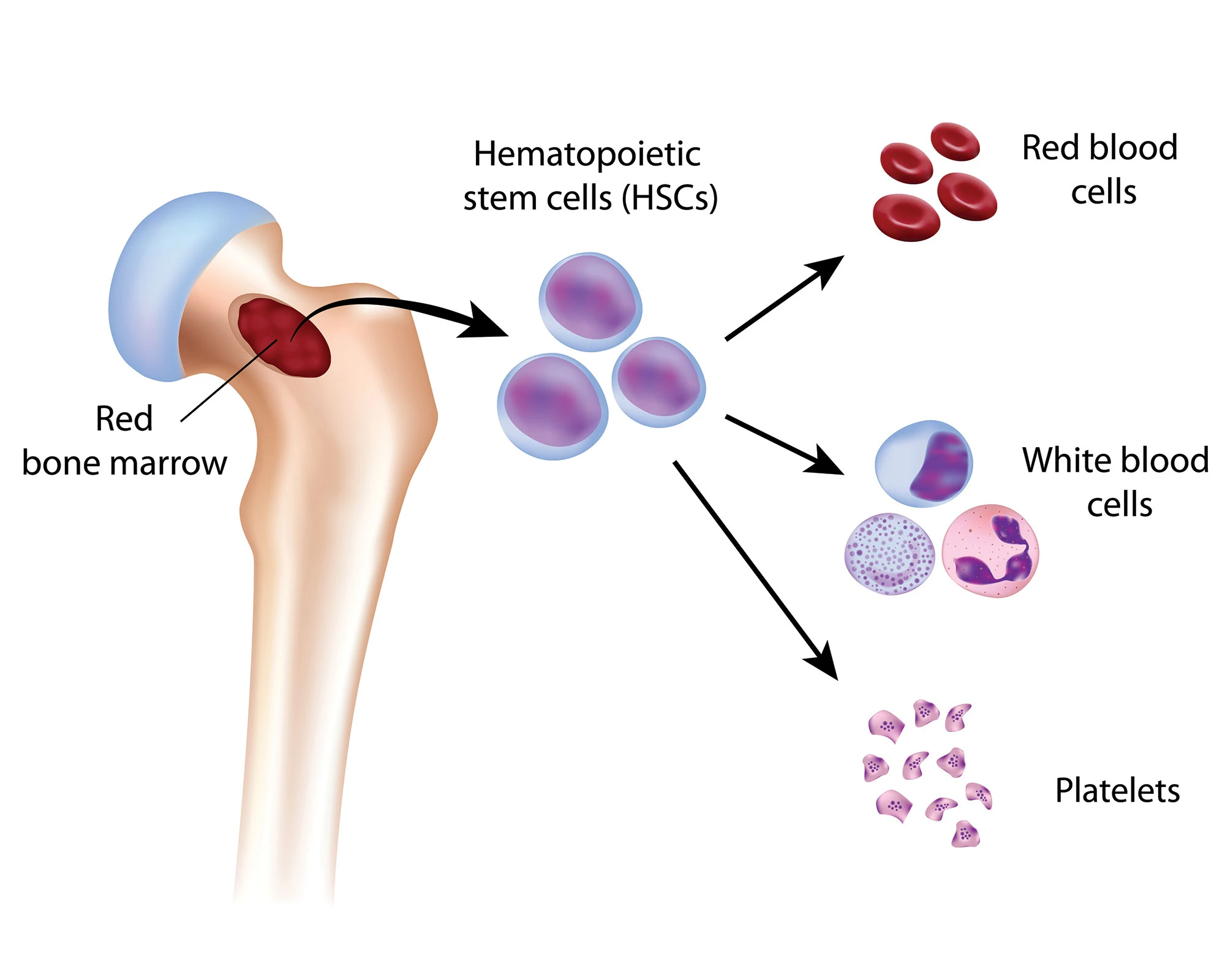
Myelodysplastic Syndromes (MDS), also known as myelodysplasia, are a group of conditions that arise from the abnormal production of blood cells in the bone marrow. The defective blood cells gradually take over the bone marrow, lowering the number of healthy blood cells – oxygen-carrying red blood cells, infection-fighting white blood cells, and platelets needed for blood clotting – in the bloodstream. MDS are considered a type of cancer.
There are different types of MDS, from the mild to more serious. MDS can also develop into a type of leukaemia (cancer of the bone marrow) called acute myeloid leukaemia (AML).
Although the exact causes of MDS are not known, there are several risk factors that may increase the likelihood of developing MDS:
- Age – The majority of cases are found in people over 60.
- Gender – MDS occurs more frequently in men than in women.
- Congenital disorders – People with certain congenital disorders, such as Down Syndrome and Fanconi anaemia, caused by mutated genes inherited from their parents may have a higher risk of developing MDS.
- Cancer treatment – Certain chemotherapy drugs or radiation therapy may increase the likelihood of developing MDS later on.
- Exposure to chemicals – Long-term exposure to industrial chemicals such as benzene, pesticides and certain petroleum products, as well as tobacco smoke, may increase the likelihood of developing MDS.
- Exposure to heavy metals – Exposure to lead and mercury have been linked to the occurrence of MDS.
- Exposure to radiation – Exposure to high doses of radiation (for example, from an atomic bomb blast or nuclear reactor accident) increases the risk of developing MDS.
Many people may experience few or no symptoms in the early stages of MDS. The condition may even be picked up accidentally during a routine blood test, which would show low blood cell counts, before any symptoms appear.
Symptoms associated with low blood cell counts include:
- Fatigue, dizziness or feeling weak, shortness of breath and looking pale as a result of having insufficient normal red blood cells (anaemia).
- Fevers, recurring or severe infections, or mouth ulcers as a result of having insufficient normal white blood cells (leukopenia).
- Bruising or bleeding easily as a result of having insufficient normal blood platelets (thrombocytopenia). Some people may experience frequent nosebleeds or bleeding gums.
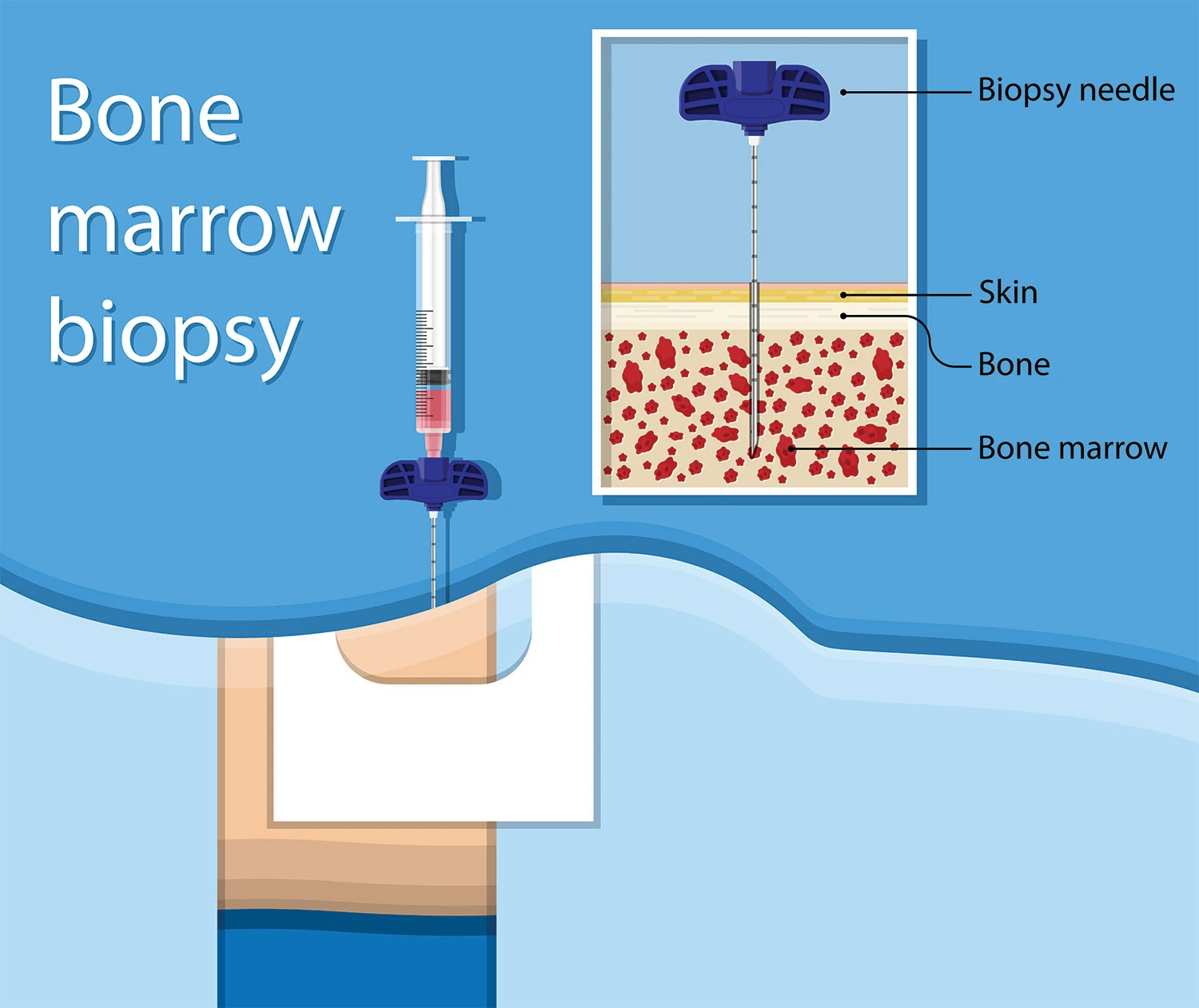
MDS is diagnosed through a blood test and bone marrow biopsy.
In the blood test, called a full blood count, a sample of blood will be sent to the laboratory for investigation. People with MDS typically have low counts of red blood cells as well as platelets, while the white blood cells will usually be abnormal.
If the blood test suggests MDS is likely, a bone marrow biopsy can help to confirm the diagnosis. A bone marrow biopsy involves taking a sample of bone marrow, usually from the hip bone. This is done under local anaesthetic and takes 15 – 20 minutes. The sample will also be sent for investigation by the laboratory, to examine the cells present and the haemopoiesis (blood forming) activity in the bone marrow.
Once MDS is confirmed, further testing on the blood and bone marrow may be done to determine the type of MDS.
For most cancers, staging or determining the stage of cancer is helpful in deciding on treatment options. As MDS are diseases of the bone marrow, the prognosis is not based on the size of a tumour or how far the cancer has spread, unlike with other cancers. Instead, MDS is scored based on various factors.
One scoring system, the revised International Prognostic Scoring System (IPSS-R), is based on the following factors:
- The percentage of blasts (very early forms of blood cells) found in the bone marrow.
- The type and number of chromosome abnormalities found in the cells.
- The level of red blood cells found in the patient’s blood.
- The level of platelets found in the patient’s blood.
- The level of neutrophils (a type of white blood cell) found in the patient’s blood.
Each factor is assigned a score, where the lowest scores correspond to the best prognosis. Adding the scores for all the factors will determine the patient’s risk group:
- Very low risk
- Low risk
- Intermediate risk
- High risk
- Very high risk
Another scoring system, the World Health Organization (WHO) Scoring System, is based on these three factors:
- The type of MDS based on the WHO classification.
- Chromosome abnormalities (which are grouped as good, intermediate, or poor).
- Whether regular blood transfusions are required.
As with the IPSS-R, each factor’s score is added up to determine the patient’s risk group.
Apart from helping to predict a patient’s prognosis, and decide on treatment options, the risk group can also predict the likelihood of MDS transforming into AML.
The treatment chosen depends on the type of MDS, risk group, age and general health of the patient. More than one type of treatment may be used simultaneously.
Monitoring
In the early stages of MDS, many people may live relatively normal lives while experiencing few symptoms. In such cases, regular check-ups to monitor the condition may suffice.
Supportive Care
Supportive care refers to the management of symptoms of MDS, and the prevention and treatment of any complications that may arise. For example, patients with MDS may need to address problems caused by low blood cell counts:
- Low red blood cell counts (anaemia) can result in symptoms such as severe fatigue. Patients may be injected with growth factor drugs to stimulate the bone marrow to make new red blood cells.
- A transfusion of red blood cells or platelets may be given as required.
- As excess iron may build up in the blood following multiple blood transfusions, drugs may be given to help the body get rid of the iron.
- Antibiotics may be given to treat infections, especially if the white blood count is low.
Chemotherapy
In chemotherapy, drugs that destroy the abnormal blood cells are given to the patient. The drugs may be administered in tablet or injection form. Chemotherapy is recommended for MDS types that may transform into AML.
Bone Marrow Transplant
A bone marrow or stem cell transplant is the only potential successful treatment for MDS. It involves destroying the abnormal blood cells using high doses of chemotherapy and replacing the abnormal blood cells with healthy donor cells. However, this treatment may not be suitable for everyone.
A mini transplant may be done instead, in which moderate doses of chemotherapy are given to destroy some abnormal stem cells in the bone marrow as well as suppress the patient’s immune response before the donated cells are transplanted.
Drug Therapies
New approaches are being developed for the treatment of MDS, such as new chemotherapy drugs, targeted therapies, biological modifiers and drugs that target the immune system.
Although MDS cannot be prevented, the following may lower the risk of developing MDS:
- Do not smoke.
- Avoid exposure to industrial chemicals such as benzene.
- Avoid exposure to heavy metals.
- Avoid exposure to radiation.
- Avoid treating cancer with radiation and chemotherapy drugs linked to an increased risk of MDS. However, some people may require these specific drugs for treatment.

CanHOPE is a non-profit cancer counselling and support service provided by Parkway Cancer Centre, Singapore. CanHOPE consists of an experienced, knowledgeable and caring support team with access to comprehensive information on a wide range of topics in education and guidelines in cancer treatment.
CanHOPE provides:
- Up-to-date cancer information for patients including ways to prevent cancer, symptoms, risks, screening tests, diagnosis, current treatments and research available.
- Referrals to cancer-related services, such as screening and investigational facilities, treatment centres and appropriate specialist consultation.
- Cancer counselling and advice on strategies to manage side effects of treatments, coping with cancer, diet and nutrition.
- Emotional and psychosocial support to people with cancer and those who care for them.
- Support group activities, focusing on knowledge, skills and supportive activities to educate and create awareness for patients and caregivers.
- Resources for rehabilitative and supportive services.
- Palliative care services to improve quality of life of patients with advanced cancer.
The CanHOPE team will journey with patients to provide support and personalised care, as they strive to share a little hope with every person encountered.
