News & Articles

Radiotherapy (Radiation Therapy): How it Works & What’s Involved?
On target
Radiotherapy is an established way of treating cancer. Parkway Cancer Centre’s Dr Edward Yang Tuck Loong looks at how it works and what’s involved.
Radiation therapy, or radiotherapy, plays a key role in the multidisciplinary approach to cancer care which also includes surgery and chemotherapy.
Radiotherapy can, in some diagnosis, play the key curative role as the primary modality in treating the tumour. It can also be used in an adjuvant or post-operative setting to enhance the control of the primary tumour and, therefore, improve the chance of long-term cure. It plays an important role in the palliation of advanced and metastatic disease in cancer.
Hence radiation therapy can be given before, during, or after other cancer treatment such as surgery, chemotherapy.
Radiotherapy uses high-energy X-rays to damage the DNA of cancer cells, thus causing tumour cells to die in the process of trying to multiply. This prevents the tumour from growing and potentially reduces its ability to spread. As it reduces the tumour size and impact, it is also effective in providing relief to symptoms like pain, bleeding and obstruction.
To minimise damage to surrounding healthy organs, radiation beams are usually aimed and “shaped” as precisely as possible, to target only the tumour or part of the organ that is affected.
With modern technological advances in engineering and digital technology, radiation beams can be shaped and modulated to conform optimally to the target it is designed to hit. Because of these advancements, the risks of collateral damage, accuracy and, therefore, the effectiveness of radiotherapy to cure cancer completely and reduce the side effects of cancer treatment, has been markedly enhanced.
Combining treatments
Radiotherapy can be used in combination with surgery, chemotherapy or immunotherapy.
For example, it can be given before surgery to shrink a tumour to make it easier to remove. It can also be given during surgery to reduce the likelihood a cancer returning; this is usually done via intraoperative radiation therapy, when radiation is delivered directly to a tumour or tumour bed during surgery, thereby sparing nearby normal tissues. Radiotherapy can also be given after surgery to kill any residual cancer cells as an adjuvant postoperative radiotherapy.
Radiation is also often combined with chemotherapy, which involves the intravenous or oral administration of drugs to impact cancer cells. These drugs may enhance the cells’ sensitivity to radiation – we call this concomitant chemoradiotherapy. Potentially the drugs “weaken” the tumour cells to radiotherapy resulting in better responses and results. This is especially seen in head and neck tumours, lung cancers and certain brain tumours as well as gynaecological cancers. Radiotherapy can also be combined with immunotherapy, an emerging form of treatment that enhances the body’s own immune system to fight cancer. As with the combination of radiation with chemotherapy or surgery, radiation therapy can be used to complement the effectiveness of immunotherapy.
Radiotherapy:
What’s involved
The process of administering radiation therapy generally involves the following steps:
Consultation: A radiation oncologist will recommend and discuss treatment options such as what type of radiation therapy to administer, how often and for how long, and the side effects. Once these are decided, a CT simulation (CT sim) appointment will then be given.
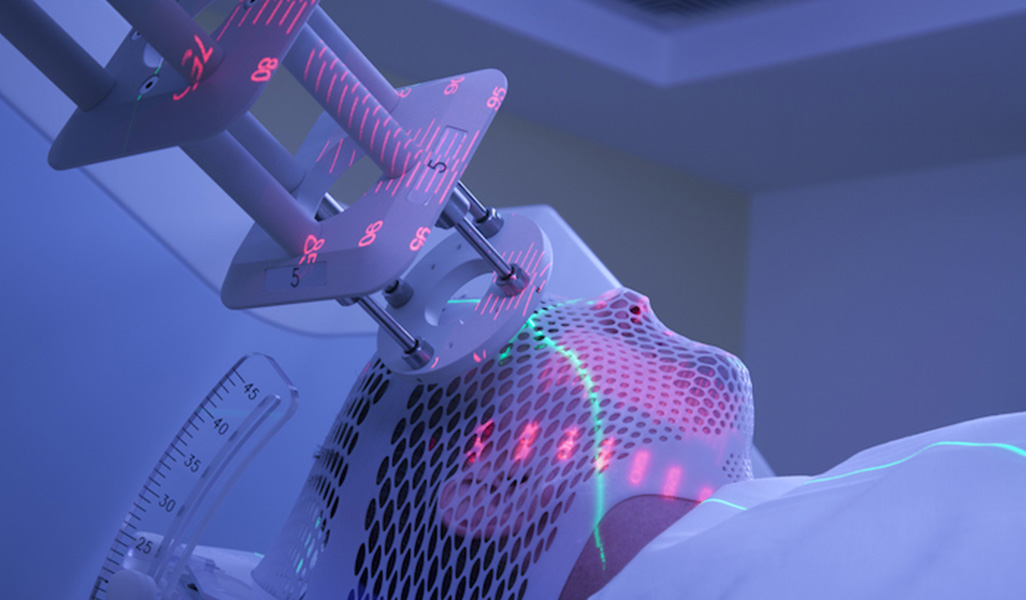
CT simulation: A CT sim is done to determine exactly how the radiation needs to be delivered, taking into account the location, shape, and size of the tumour. The positioning, immobilisation technique and anatomical region are decided upon at this procedure so that the radiotherapy treatment planning can be implemented.
Treatment planning: CT images taken from the CT sim are used to accurately predict how the radiation dose will be deposited in the patient’s body, which enables the radiation oncologist to determine how to treat the tumour with as little side effects as possible. Adjacent and intervening organs at risk (critical organs) are avoided as far as possible and the dose to them are limited in the plan that will be subsequently developed. The radiation oncologist will ensure that localisation of the target volume and safety treatment margins are adequate.
This is then passed on to the Medical Physicist or Dosimetrist who will develop various approaches (plans) to irradiate the tumour safely and will discuss it with the Radiation Oncologist who will finally decide as to the best option to ensure best dose distribution to the tumour as well as safety and minimal risk to adjacent tissue. Before the chosen plan for treatment is implemented, a quality assurance test is done using a model which helps ensure the plan is accurate and deliverable.
Daily treatment: On confirming the quality assurance of the plan, the radiation therapy can then start. Whilst on treatment, image guidance is also implemented, be it with cone-beam CT or electronic portal imaging, so as to ensure daily accuracy of the delivered plan. Moreover, in some cases, when there is a marked change in tumour size or shape of the patient due to weigh loss or gain, another CT sim and re-planning of the treatment may be needed to ensure continued patient safety and accuracy of the delivered radiation. During the treatment course, regular consultations will be held so that the patient’s treatment progress can be reviewed and discussed.
Follow-up consultation: After treatment is completed, doctors will see the patient for a follow-up consultation. The follow-up will be a team effort of the other doctors involved. This will also include subsequent imaging and blood tests where necessary.
Radiotherapy: What you can do
If you’re going to undergo radiotherapy, here’s what you need to do:
Get plenty of rest: While you can continue working while undergoing radiotherapy, do monitor your condition closely and let your doctor know if you feel especially tired or uncomfortable. It is important to get enough rest, as it will make your recuperation more effective.
Maintain a positive outlook: Get support from family and friends to go through the treatment. If you’re struggling with distress, anxiety or depression, it is highly recommended to seek help from professional counselling.
Have a balanced diet: Maintaining good nutrition will help you cope with the strains of radiotherapy.
Stay hydrated: Drink plenty of fluids to help your body heal effectively.
Protect your skin: Your skin is likely to be more sensitive after radiation. Use moisturisers that are free from perfumes and parabens to minimise irritation and practise good personal hygiene to keep the treatment area clean and free from infection.
Cope with side effects: General side effects from radiotherapy include nausea, thirst and fatigue. The more specific side effects will depend on the area of treatment. They may occur but with more sophisticated radiotherapy techniques, there’s a lot less side effects today. Typical side effects for:
- Cranial radiation: Headache, nausea, giddiness, double vision and other neurological symptoms, temporary hair loss.
- Head and neck radiation: Mucositis and loss of taste, mouth dryness and excessive mucoid saliva, sore throat, pain on swallowing, loss of voice, skin reactions.
- Thoracic radiation: Cough, uncomfortable swallowing, voice hoarseness.
- Abdominal and pelvic radiation: Gastritis, colic and wind in the gut, diarrhoea, slight pain and frequency of urination.
- Breast irradiation: Slight breast pain, mild skin reactions.
If you’re pregnant or are worried about fertility
The effects of radiation on fertility depends on the type of cancer being treated. For example, radiation therapy for breast cancer patients will not affect fertility, but treatments for cancers in the abdomen, cervix and pelvis will affect fertility. It is important not to become pregnant until treatment is completed, as the radiation may affect the foetus. And if you’re planning to have kids, talk to your doctor to get a better understanding on the possible side effects of radiation therapy on fertility and pregnancy.
Written by Kok Bee Eng
| TAGS | cancer & pregnancy, common side effects of cancer treatment, immunotherapy, radiotherapy (radiation therapy), tumours |
| READ MORE ABOUT | Breast Cancer, Lung Cancer |
| PUBLISHED | 15 August 2019 |
