News & Articles

Breast Cancer Screening: Why Bother?
Screen early, screen often
Breast cancer is the no. 1 cancer among women in the world. In Singapore, 2,000 women are diagnosed with breast cancer every year. Early detection through screening, however, can improve the chances of survival.
Screening: Why bother?
Dr Wong Chiung Ing from Parkway Cancer Centre talks about the importance of early detection of breast cancer in women.
Breast cancer is the most common cancer among women around the world, including Singapore. According to the World Health Organization International Agency for Research on Cancer, an estimated 1.67 million new breast cancer cases are diagnosed per year, accounting for 25 per cent of all cancers.
Closer to home in Singapore, breast cancer constitutes 30 per cent of all cancer diagnoses in women, with an estimated 2,000 new cases diagnosed per year.
The risk of breast cancer increases with age, with the highest incidence rate of diagnosis seen among women aged between 50 and 59 years. Survival rates, however, are generally improving as a result of earlier detection and better treatment methods.
Screening usually involves checking your breasts for cancer even before there are any signs and symptoms. While screening cannot prevent breast cancer, it can help you to detect the cancer early, so that it can be treated earlier. Talk to your doctor about which screening tests to do and when you should do them. In general, screening tests include:
Mammogram
This is the most common and primary screening tool for detecting breast cancer. It detects changes such as abnormal densities or calcium deposits in the breasts.
As the procedure involves having the breasts compressed to spread the tissue so that small abnormalities are not obscured, some women may find mammograms uncomfortable or painful. But these two minutes or so of discomfort could save your life.
What’s involved? In a mammogram, low-dose X-rays are used to create images of the breast. The radiographer will position each breast in the mammography unit and compress it for a few seconds to take different views of each breast.
It is recommended that you go for a mammogram when your breasts are the least tender, which is usually about a week following your period.
Depending on the mammogram results, the doctor may recommend further tests such as another mammogram to take different views of your breasts, and a breast ultrasound scan to examine the breast tissue.
When should you go? Women above 40 years old should go for a mammogram every year, while those above 50 years old should do it every two years.
Ultrasound scan
An ultrasound scan is a supplemental test for women with very dense breasts, which make it difficult for a mammogram to detect small abnormalities. It can tell between a solid mass (which may be cancerous) and a fluid-filled cyst (which is usually not cancerous).
When done in addition to a mammogram and breast self-examination, it can help the doctor decide if more tests such as a biopsy is needed. However, while it may be less painful than a mammogram, an ultrasound scan should never be used to replace a mammogram, and vice-versa.
What’s involved? Ultrasound scans use high-frequency sound waves instead of X-rays and are safe for pregnant women and mothers who are breastfeeding. A gel is put on the skin of the breast, followed by moving a small hand-held probe across the breasts to produce detailed images of the inside of the breasts. The scan usually lasts between 10 and 30 minutes.
When should you go? Women above 40 years old can do both a mammogram and ultrasound scan as part of their annual screening. Those above 50 can include an ultrasound scan during their two-yearly mammography screening. Check with your doctor on whether an additional test of ultrasound scan is needed or not.
Breast MRI
MRI, or magnetic resonance imaging is a scan that is usually used in further evaluation of patients who have been diagnosed with breast cancer. For certain women at high risk of breast cancer (either because of a very strong family history or a gene abnormality), a MRI screening is recommended along with a yearly mammogram.
What’s involved? MRI uses radio waves and strong magnets to make detailed, cross-sectional pictures of the breast. You will need to lie on your stomach on a motorised table with cushioned openings for your breasts. Each opening is surrounded by breast coil which is a signal receiver to help create the images. The scan takes about 30 to 45 minutes. You will hear a loud noise whilst in the MRI machine and if you are claustrophobic, you may find the scan difficult to tolerate.
When should you go? Breast MRI can only be recommended by doctors after determining if the woman is at high risk for breast cancer. It is not recommended as a screening test for women at average risk of breast cancer.
Breast self-examination (BSE)
Examining your breasts on your own regularly is an important step you can take to detect breast cancer early.
What’s involved? Take these steps for a self-examination. The best time to examine your breasts is the week after your period ends, when the breasts are least likely to be swollen and tender.
When should you do this? Monthly breast self-examination starting by age 25 is recommended. Clinical breast examination by a trained medical professional at least every three years starting at age 25, and annually after 40 years old.
Risk factors
Studies have shown that the risk of getting breast cancer depends on a combination of factors. Having one or more risk factors does not mean you will get the cancer, but being aware of them can help you to take protective steps to reduce the risk. They include:
- Family history
- Certain inherited genes
- History of malignant or benign (non-cancerous) breast disease
- Early onset of menstruation
- Late menopause
- Having first child after the age of 35
- Having fewer children or never had children
- Being on hormone replacement therapy
- Drinking too much alcohol
- Being overweight or obese
It is possible to get breast cancer even if you have none of these risk factors.
Regular screening and breast self-examination are thus important, as you may not see any symptoms of early-stage cancer, such as a lump, nipple inversion, unusual discharge, ulceration, pain, or skin changes on the breast and nipple.
You can also reduce your risk through lifestyle choices such as maintaining a healthy weight by having a balanced diet, exercising regularly, limiting your intake of alcohol, and not smoking (or quitting if you smoke).
Breast cancer survival rates have improved as a result of advancement in surgical procedures, the availability of effective chemotherapeutic agents, and breakthroughs in targeted therapy. However, the best weapon against breast cancer is still awareness: Know your body, know your risks and early detection.
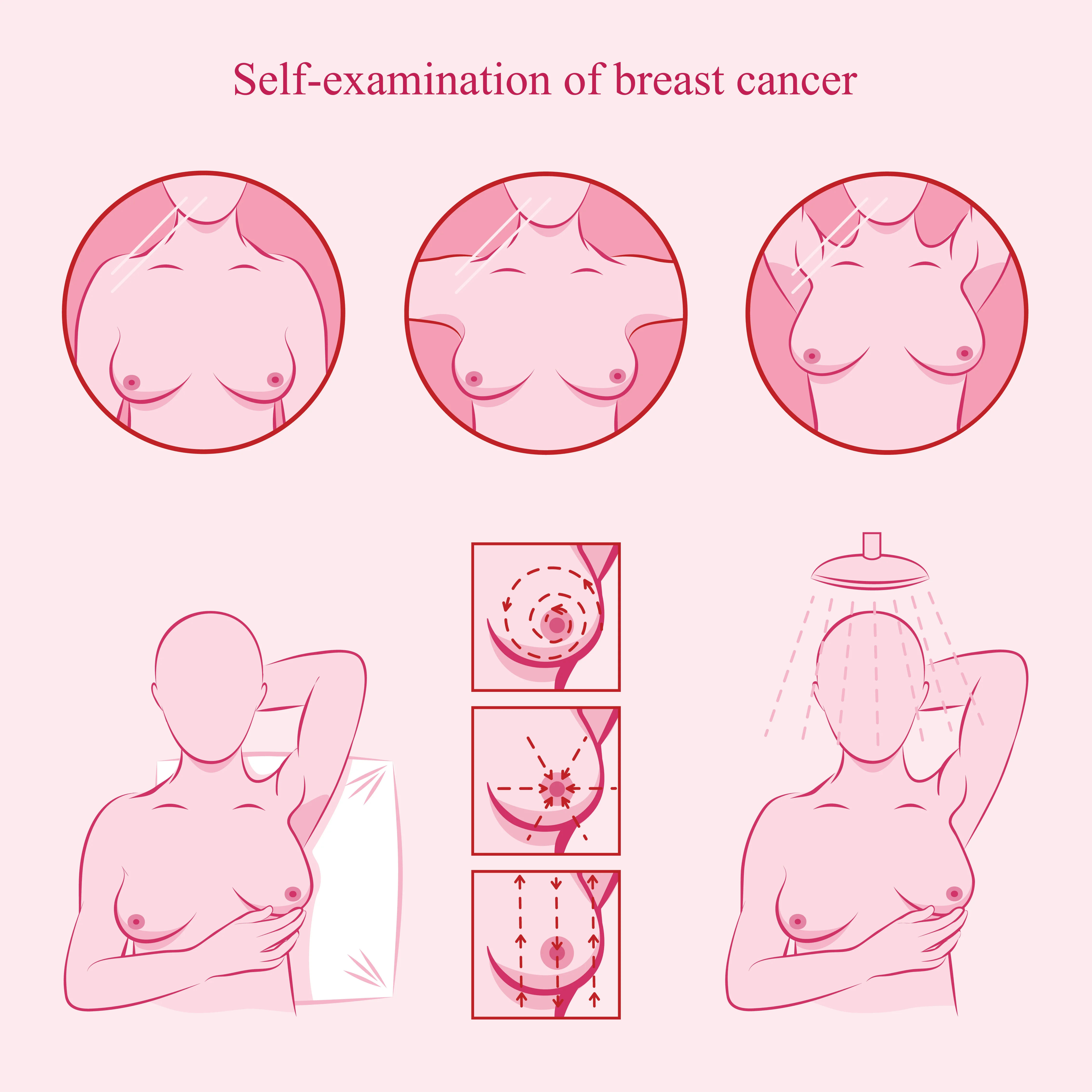
Breast self-examination: What to do
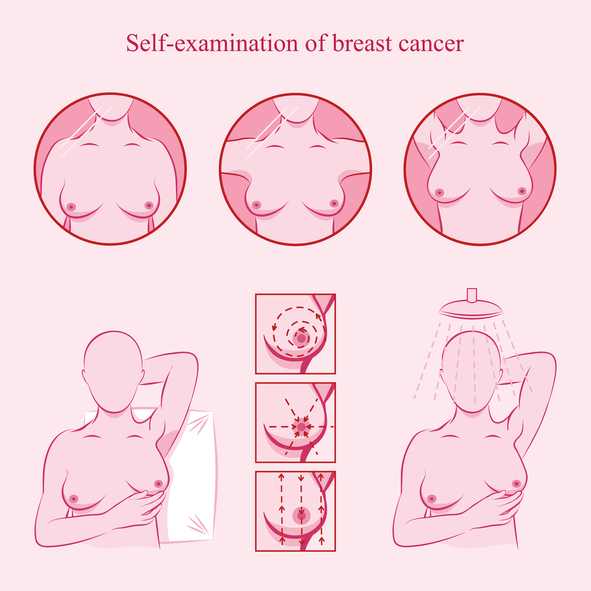
- Look into a mirror, keeping your shoulders straight and your arms on your hips. Check your breasts and nipples for any rash, redness, swelling or changes such as a nipple that has become inverted (pushed inward instead of sticking out).
- Still in front of the mirror, raise your arms and look for the same changes as in step (1).
- Squeeze each nipple gently to see if there is any discharge such as a watery, milky, or yellow fluid or blood.
- Lie down and feel each breast. Keeping your fingers flat and close together, use your right hand to feel the left breast and vice-versa. Use a circular motion from top to bottom and side to side – from collarbone to abdomen, from armpit to cleavage. Begin with a soft touch, and increase pressure to feel the deeper tissue. Cover the entire breast.
- Do the same as in step (4) while standing or sitting.
Screening:
When and what
If you are...
Over 25 years old:
- Monthly breast self-examination (BSE)
40-49 years old:
- Monthly BSE
- Yearly mammogram +/- ultrasound scan
50 years old and above:
- Monthly BSE
- Mammogram +/- ultrasound scan every two years
| POSTED IN | Cancer Prevention |
| TAGS | cancer screening, cancer self-examination, cancer ultrasound, history of cancer, mammogram, reduce cancer risk, women (gynaecological) cancer |
| READ MORE ABOUT | Breast Cancer |
| PUBLISHED | 08 October 2018 |
