Ovarian Cancer
Overview
What is Ovarian Cancer?
Ovarian cancer is a disease where abnormal cells in your ovaries or fallopian tubes grow out of control and form a tumour (mass). The ovaries are part of a woman’s reproductive system, where the eggs develop and female hormones (oestrogen and progesterone) are produced. The fallopian tubes are the passage through which the eggs travel from the ovaries to the uterus (womb).
Types of Ovarian Cancers
Ovarian cancer is categorised based on the type of cell where the cancer originated from1,2:
- Epithelial ovarian cancer: This type arises from the outer surface (epithelium) of the ovary and accounts for around 90% of ovarian cancers3. It includes several subtypes, including serous, endometrioid, clear cell, mucinous and undifferentiated carcinomas.
- Stromal tumours: These rare tumours arise from the supporting cells in the ovaries that produce hormones. They are usually diagnosed at an earlier stage than other ovarian cancers and generally have a good outlook.
- Germ cell tumours. These rare ovarian cancers occur in the cells that produce the eggs (germ cells) and tend to occur in younger women. The outcome following treatment is usually good.
How Common is Ovarian Cancer?
Ten most frequent cancers and cancer deaths in Singapore
Ovarian cancer is the sixth most common cause of cancer, accounting for 4.3% of all cancer cases diagnosed in Singapore4. It is also the sixth leading cause of cancer deaths4. The number of cases has increased more than twofold over the past fifty years, possibly due to changes in reproductive patterns including delayed childbearing and having fewer children, increased use of hormone replacement therapy and lifestyle factors such as reduced physical activity5.
Causes & Symptoms
What causes Ovarian Cancer?
Ovarian cancer happens when cells in the ovary or fallopian tube develop changes (mutations) in their DNA that cause the ovarian cells to grow abnormally and develop into a tumour. The exact trigger for the mutations is not fully known.
Ovarian Cancer Risk Factors
While the exact cause of ovarian cancer remains unknown, factors that may increase the risk of ovarian cancer include1,2,6:
Older age: Ovarian cancer is rare in women aged under 40 years. Most ovarian cancers develop after menopause7, with the highest risk seen in those aged between 75 to 79 years6. Older age at diagnosis is also associated with a poorer outcome.
Inherited gene changes: A small percentage (around 5 to 15%6) of ovarian cancers are caused by genetic mutations (changes) that are passed from generation to generation.
Mutations in BRCA1 or BRCA2 genes account for the majority of hereditary ovarian cancers7. Women who have these mutations have up to a 70% chance of getting ovarian cancer during their lifetime7. These faulty genes also increase the risk of other cancers such as breast, uterine (womb), pancreatic and prostate cancers.
Other rare inherited conditions such as hereditary nonpolyposis colorectal cancer (HNPCC, also known as Lynch syndrome) and Peutz-Jeghers syndrome are caused by mutations in other genes and are associated with increased risk of multiple cancers, including ovarian cancer.
Family history of ovarian cancer: Women with a first-degree relative (mother, sister or daughter) diagnosed with ovarian cancer have around three times the risk of ovarian cancer compared to someone without a family history6.
Never been pregnant or being pregnant later: Having children appears to reduce the risk of ovarian cancer, and the more children you have, the lower the risk. Breastfeeding may also reduce the risk further. This protective effect is thought to be due to fewer ovulations over the woman’s lifetime, as ovulation (the process where eggs are released from the ovary) does not happen during pregnancy and breastfeeding. The fewer times you ovulate in your lifetime, the lower the risk of ovarian cancer6. Women who become pregnant for the first time after age 35 have a higher risk of ovarian cancer compared to women who were pregnant at a younger age7.
Age when menstruation started and ended: Beginning menstruation at an early age or starting menopause at a later age, or both, may increase the risk of ovarian cancer as it increases the number of menstrual cycles (causing ovulation) over your lifetime.
Postmenopausal hormone replacement therapy: Taking hormone replacement therapy to control menopause symptoms may increase the risk of ovarian cancer, especially if used for more than five years2.
Previous breast cancer: Breast cancer survivors, especially those diagnosed at a younger age or have family members who also had breast cancer, have an increased risk of developing ovarian cancer6. These cancers have common hormonal and reproductive risk factors.
Endometriosis: Endometriosis is a condition in which tissue that normally lines the inside of the uterus grows outside the uterus. It increases the risk of clear cell and endometrioid ovarian cancers.
Smoking: Smoking increases the risk of certain types of ovarian cancer such as mucinous ovarian cancer.
Being overweight or obese: Carrying excess body weight, especially in early adulthood is associated with an increase in the risk of ovarian cancer2.
Having one or more of these risk factors does not automatically mean that you will get ovarian cancer. Many people with risk factors never develop ovarian cancer, whilst some with no known risk factors do.
What are the Signs and Symptoms of Ovarian Cancer?
This cancer has few or no symptoms in the early stages, which makes early detection difficult. When they do occur, signs and symptoms of ovarian cancer may include1:
- Abdominal (belly) bloating or discomfort.
- Changes in bowel habits, such as constipation.
- Frequent need to urinate.
- Loss of appetite, feeling full quickly.
- Pain in the pelvic area.
- Pain during sexual intercourse.
- Back pain.
- Unintentional weight loss.
- Persistent tiredness that is not relieved with rest.
Most of these symptoms are more likely to be caused by more common ailments such as an infection or gut issues. However, if you have any of these symptoms, especially if they persist or get worse, you should see a doctor to have it checked out and treated if needed.
Diagnosis & Assessment
Diagnosis of Ovarian Cancer
If ovarian cancer is suspected, your doctor will investigate further to determine if you have cancer1,8,9:
Clinical history and examination: Your doctor will ask about symptoms, risk factors and family history as well as perform a physical and pelvic examination. During a pelvic examination (also known as vaginal or internal examination), your doctor will check the inside of the vagina and cervix to look for any abnormalities. The size and shape of the uterus and ovaries will also be assessed for any tenderness or enlarged areas.
Blood tests: Blood tests can measure certain proteins called tumour markers that are produced by cancer cells. One tumour marker test used in ovarian cancer diagnosis is called CA-125. However, it is not always accurate for diagnosis of ovarian cancer as some ovarian cancers do not make CA-125 and it can also be raised in non-cancerous conditions, such as endometriosis and appendicitis. If your doctor suspects germ cell cancer, other tumour markers may be checked, including human chorionic gonadotropin (HCG), alpha-fetoprotein (AFP), and lactate dehydrogenase (LDH). Other blood tests are also done to check your general health and how your kidneys and liver are functioning.
Imaging tests: Imaging tests take detailed pictures that show the inside of the body. Tests used to diagnose ovarian cancer include ultrasound, computed tomography (CT) scan, Magnetic resonance imaging (MRI) scans and positron emission tomography (PET) scans of the abdomen. They can show the size and position of a tumour, blood vessels and whether the cancer has spread elsewhere.
Tissue sampling:
Biopsy is the removal of tissue samples to be viewed under a microscope to check for signs of cancer. For ovarian cancer, the biopsy is most often obtained by removing the tumour during surgery. In rare situations, a suspected ovarian cancer may be biopsied during a laparoscopic procedure (a minimally invasive surgical procedure using a camera and instruments inserted through small cuts in the abdomen) or with a needle placed directly into the tumour through the skin of the abdomen under ultrasound or CT scan guidance. This is usually only done if you cannot have surgery because of advanced cancer or are unfit for surgery due to other serious medical condition, as there is concern that a biopsy could spread the cancer.
If you have ascites (fluid build-up inside the abdomen), samples of the fluid obtained via a needle through the abdominal wall with ultrasound guidance or during surgery can also be used to diagnose the cancer. The tissue biopsy or fluid is analysed in a laboratory to determine whether cancer cells are present, and if so, what type of ovarian cancer and grade it is (how abnormal the cells look under the microscope).
In addition, genetic testing may be done to look for specific genes, proteins and other substances (called biomarkers or tumour markers) that the cancer cells might have. The presence of these genetic mutations can guide cancer treatment selection.
How is Ovarian Cancer Assessed?
After ovarian cancer has been diagnosed, your doctor will determine the extent (stage) of the disease. Staging is done to find out whether the cancer has spread, and if so, to what parts of the body. Imaging tests such as CT scans, PET-CT scans or MRI can give an idea of the stage of the cancer. However, your doctor may only be able to ascertain the exact stage at the time of surgery. Ovarian cancer spreads most often to nearby lymph nodes, bladder, uterus and rectum, and then to the peritoneum (the lining of your abdominal cavity), bowel, stomach, liver and lungs. Unfortunately, the majority of ovarian cancers have already spread beyond the ovaries by the time they are diagnosed.
The stages of ovarian cancer are10:
- Stage I: The cancer is only in the ovary or fallopian tube.
- Stage II: The cancer has grown outside the ovaries into the pelvic area.
- Stage III: The cancer has spread outside the pelvis to the lining of the abdominal cavity (peritoneum). It may also have spread to the lymph nodes in the back of the abdomen.
- Stage IV: The cancer has spread to other organs some distance away from the ovaries, such as the liver or lungs.
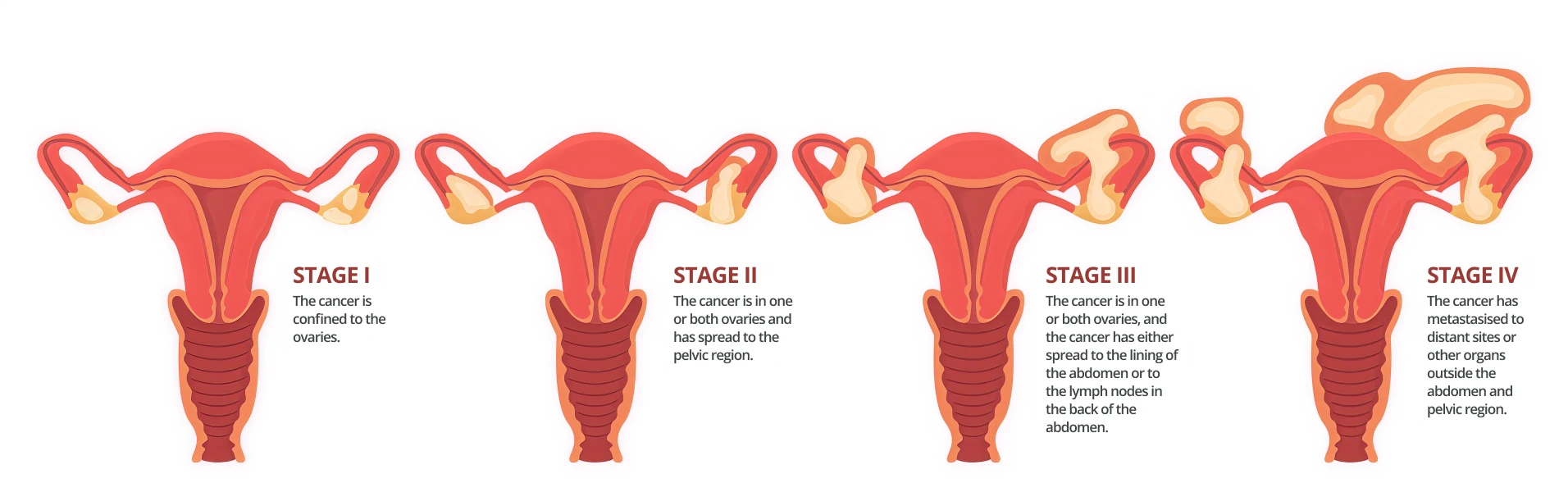
The lower the stage at diagnosis, the higher the chance of successful treatment and long-term survival.
Treatment
Ovarian Cancer Treatment Options
When considering your treatment plan your doctor will consider the following factors11:
- The stage (extent) of the disease.
- Characteristics of the tumour (which type, subtype and grade the cancer is).
- Your age, overall health and any other treatments you may have for other illnesses.
- Whether you want to be able to have children.
- Your preferences.
The first goal of ovarian cancer treatment is to get rid of the cancer. When that is unachievable, the focus may be on stabilising the cancer to prevent its progression for as long as possible and improving quality of life. Ovarian cancer can be treated with the following methods, often used in combination1,12,13,14:
Surgery: To determine the actual extent of the cancer, surgical exploration or staging is required. During the procedure, the doctor will examine the peritoneum, which is the inner lining of the abdomen. Biopsies (sampling) of lymph nodes and different areas inside the abdominal and pelvic cavities as well as any fluid in the cavities are collected and sent to the laboratory for analysis under a microscope to look for cancer cells.
The other important part of surgery is to remove as much of the tumour as possible. Most women would have a hysterectomy (removal of the uterus), salpingo-oophorectomy (removal of both ovaries and fallopian tubes), and lymph node dissection (removal of lymph nodes). If the cancer has spread throughout the pelvis and abdomen, a debulking procedure to remove as much of the cancer as possible may be done.
If you have early, low-grade cancer and wish to have children after treatment, you may potentially be given the option to remove only the ovary containing the cancer along with the fallopian tube on the same side. This leaves behind the unaffected ovary and uterus (womb) thereby making pregnancy possible.
For very early-stage disease and non-aggressive cancer types, surgery will likely cure the cancer and further treatment may not be required. For more advanced and aggressive types of cancers, chemotherapy after (and sometimes also before) surgery is needed.
Chemotherapy: Chemotherapy is the use of anti-cancer (cytotoxic) drugs to kill cancer cells or stop them from dividing. It can be given through a vein (intravenous) or taken by mouth (oral), where it then circulates through the bloodstream to reach almost all areas of the body. It is commonly used after surgery for high grade and advanced cancers to kill any cancer cells that might remain. It may also be used before surgery to shrink the tumour to make surgery easier. Sometimes, chemotherapy drugs may be heated and infused through a catheter (thin tube) directly into the abdomen (known as hyperthermic intraperitoneal chemotherapy).
Targeted therapy: Targeted therapies are drugs that block the growth of cancer by interfering with specific molecules present in cancer cells that are involved in tumour expansion and spread. Targeted therapy tends to cause less harm to normal cells than chemotherapy or radiation therapy do, due to its specific action on cancer cells. It is usually combined with chemotherapy for treating advanced ovarian cancers which have specific genetic mutations.
Immunotherapy: Immunotherapy is treatment that boosts the body’s immune system to fight the cancer. This can be done by genetically engineering your own immune cells to fight endometrial cancer cells, or using medications that help your immune system cells identify and attack the cancer cells. Immunotherapy is used in the treatment of certain advanced ovarian cancers with specific genetic mutations.
Hormonal therapy: Hormonal therapy is a cancer treatment that blocks the effects of oestrogen on some types of ovarian cancers that rely on oestrogen to help them grow.
Radiation therapy (Radiotherapy): Radiation therapy is the use of powerful, high-energy beams to kill cancer cells or keep them from growing. It is rarely used to treat ovarian cancer.
Ovarian Cancer Survival Rate
The overall 5-year relative survival rate across all ovarian cancer cases in Singapore is around 43%4. However, the earlier the cancer is detected and treated, the higher the likelihood for cure. Around 45% of ovarian cancers are diagnosed in Stage I4, which has close to 90% 5-year relative survival rate15.
Unfortunately, about 20% of patients are diagnosed with advanced (Stage IV) ovarian cancer4 and the prognosis for this group is significantly less favourable, with a survival rate of 19%15. It is worth noting that survival rate statistics are measured every 5 years and therefore may not reflect the recent advances in ovarian cancer treatment. People who are diagnosed with advanced ovarian cancer now are likely to have a better prognosis (outcome) than these numbers indicate.
Survival rates are grouped based on stage (how far the cancer has spread), but other factors such as the type and grade of the cancer, your age, overall health and how well the cancer responds to treatment can also affect your prognosis (outcome). Even taking these things into account, the prognosis your doctor gives you will be an estimate based on the statistics we have of people who have had the same diagnosis. Your journey may still differ from another person’s in a similar situation.
Prevention & Screening
Ovarian Cancer Screening
Screening refers to looking for cancer before a person has any symptoms. There is currently no routine screening test recommended for ovarian cancer. This is because there is no test that reliably picks up ovarian cancer at an early stage16. However, women who have inherited genetic conditions such as BRCA gene mutations, Lynch syndrome or a strong family history of ovarian and breast cancers have a high risk of developing ovarian cancer and should be monitored closely.
Ovarian Cancer Prevention
While there is no guaranteed way to prevent ovarian cancer, there are some measures you can take to reduce your risk1,17,18:
Consider taking oral contraceptives: Taking oral contraceptives (birth control pills) reduces the risk of ovarian cancer. Women who used oral contraceptives for five or more years have about a 50% lower chance of developing ovarian cancer compared with women who have never used oral contraceptives18. But these medications do have some serious risks and side effects, including a slightly increased risk of breast cancer. You should discuss with your doctor whether this option is right for you.
Weigh up the risks and benefits of hormone replacement therapy after menopause: Like any other medicine, oestrogen treatment for menopausal symptoms should be used at the lowest dose required and for the shortest time possible. Regular follow-up and pelvic examination are recommended whilst you remain on hormone replacement therapy.
Consider genetic counselling and testing: If you have a strong family history of breast and ovarian cancers, or inherited genetic conditions that put you at high risk of ovarian and other cancer, discuss with your doctor about the possible benefits of genetic counselling and testing. If you are found to have a genetic mutation such as BRCA mutation, you may be recommended surgery to remove your ovaries and fallopian tubes before they become cancerous. Premenopausal women who have BRCA gene mutations and have had their ovaries removed reduce their risk of ovarian cancer by 85 to 95% as well as their risk of breast cancer by 50% or more18.
Maintain a healthy lifestyle: Staying active and exercising regularly improves your overall health and wellbeing. Try to exercise most days of the week. If you are new to exercise, start slow with a gentle activity such as a walk around the park, and work your way up gradually. Eating a healthy, balanced diet with less fat, sugar, red meat and highly processed foods, and more fresh fruits, vegetables and whole grains can help to reduce the risk of many diseases and cancers. If you smoke, talk to a member of your health care team about ways to help you stop. These might include support groups, medicines and nicotine replacement therapy.
Frequently Asked Questions (FAQ)
Ovarian cancer and its treatment(s) can alter your relationship with food. You may have loss of appetite, nausea, vomiting, mouth ulcers causing difficulty chewing and indigestion which could affect your food intake. You might find making certain changes to your diet helpful, such as:
- Avoiding nutrient-poor foods: Where possible, choose healthy, nutrient-dense food options instead of empty calories/nutrient-poor foods such as sugary drinks, packaged snacks and carbohydrate-based desserts.
- Avoiding large meals: If you have poor appetite, try eating six smaller meals a day instead of having three larger meals.
- Avoiding foods that cause indigestion: Foods such as fizzy drinks, alcohol, spicy food, pickles, citrus fruits and caffeine can cause indigestion.
- Having a healthy and balanced diet: A balanced diet with more fruits, vegetables and whole grains, and less preserved food, red meat and processed meats reduces the risk for cancers other than ovarian cancer too.
Some cancer treatments can weaken your immune system, making you more susceptible to common illnesses such as the flu and COVID-19. They may also cause you to feel easily tired. You may need to make some changes to your lifestyle, including:
- Avoiding crowded places: As much as possible, stay away from very crowded, poorly ventilated places. If you must be there, maintain contact precautions such as wearing a mask, keeping your distance and washing your hands.
- Allowing yourself time to rest: You may find that you tire a lot more easily and are unable to sustain an activity for extended periods. Allow yourself extra time to complete an activity and avoid doing too much in a day. Ensure that you have periods of rest in between.
Having a cancer diagnosis can be confronting. You may experience changes in your mood such as feeling anxious, depressed or hopeless, which in turn may affect your outlook and thoughts about your future. Avoid keeping these feelings to yourself. If you find that your mood is persistently low or you are withdrawing from activities or social contact that you would previously have enjoyed, speak to your doctor. Joining a support group where you get to meet others with a similar diagnosis can be of great benefit.
Ovarian cancer that is diagnosed early (Stage 1) has a high chance of a good outcome. About 90% of women with Stage I ovarian cancer are potentially cured following treatment with surgery and if required, chemotherapy.
Ovarian cancer can take years to develop without causing any symptoms. However, once symptoms show, it can progress quickly. High grade ovarian cancers tend to grow and spread faster than slow grade cancers. Almost half of all ovarian cancers are diagnosed after the cancer has spread.
Some stromal and germ cell ovarian cancers (see Types of Ovarian Cancer above) are fully contained in one ovary and surgery to remove the affected ovary may provide a cure. However, more often a more extensive surgery, involving the removal of both ovaries, fallopian tubes, uterus and lymph nodes, is required to ensure all cancer is removed. Chemotherapy may be required following surgery to kill any potential remaining cancer cells.
The most significant risk factor for ovarian cancer is an inherited genetic mutation in BRCA1 or BRCA2 genes. Inherited mutations in these genes account for about 5 to 15 percent of all ovarian cancers6. Women who have these mutations have up to a 70% chance of getting ovarian cancer during their lifetime7. Due to the high risk of developing breast cancer, surgery may be recommended to remove the ovaries and fallopian tubes before they become cancerous. If you or a family member are known to have these genes, you should consider genetic counselling to discuss this further, in relation to your personal circumstance.
References
- Mayo Clinic. Ovarian Cancer. Accessed at https://www.mayoclinic.org/diseases-conditions/ovarian-cancer/symptoms-causes/syc-20375941 on 08 July 2024.
- Gleneagles Hospital. Ovarian Cancer. Accessed at https://www.gleneagles.com.sg/conditions-diseases/ovarian-cancer/symptoms-causes on 08 July 2024.
- Cancer Research UK. Epithelial Ovarian Cancer. Accessed at https://www.cancerresearchuk.org/about-cancer/ovarian-cancer/types/epithelial-ovarian-cancers/epithelial on 08 July 2024.
- National Registry of Diseases Office. Singapore Cancer Registry Annual Report 2021. Singapore, National Registry of Diseases Office; 2022.
- National Registry of Diseases Office. Singapore Cancer Registry 50th Anniversary Monograph. Singapore, National Registry of Diseases Office; 2022.
- Cancer Research UK. Risks and Causes of Ovarian Cancer. Accessed at https://www.cancerresearchuk.org/about-cancer/ovarian-cancer/risks-causes on 08 July 2024.
- American Cancer Society. Ovarian Cancer Risk Factors. Accessed at https://www.cancer.org/cancer/types/ovarian-cancer/causes-risks-prevention/risk-factors.html on 08 July 2024.
- Cancer Research UK. Tests for Ovarian Cancer. Accessed at https://www.cancerresearchuk.org/about-cancer/ovarian-cancer/getting-diagnosed/tests-ovarian-cancer on 08 July 2024.
- American Cancer Society. Tests for Ovarian Cancer. Accessed at https://www.cancer.org/cancer/types/ovarian-cancer/detection-diagnosis-staging/how-diagnosed.html on 08 July 2024.
- Cancer Research UK. Stages and Grades of Ovarian Cancer. Accessed at https://about-cancer.cancerresearchuk.org/about-cancer/ovarian-cancer/stages-grades on 08 July 2024.
- Cancer Research UK. Stage I Ovarian Cancer. Accessed at https://about-cancer.cancerresearchuk.org/about-cancer/ovarian-cancer/stages-grades/stage-1 on 08 July 2024.
- Cancer Research UK. Treatment Decision for Ovarian Cancer. Accessed at https://about-cancer.cancerresearchuk.org/about-cancer/ovarian-cancer/treatment/treatment-decisions on 08 July 2024.
- American Cancer Society. Surgery for Ovarian Cancer. Accessed at https://www.cancer.org/cancer/types/ovarian-cancer/treating/surgery.html on 08 July 2024.
- American Cancer Society. Chemotherapy for Ovarian Cancer. Accessed at https://www.cancer.org/cancer/types/ovarian-cancer/treating/chemotherapy.html on 08 July 2024.
- National Registry of Diseases Office. Singapore Cancer Registry 50th Anniversary Monograph – Appendices. Singapore, National Registry of Diseases Office; 2022.
- Cancer Research UK. Screening for Ovarian Cancer. Accessed at https://about-cancer.cancerresearchuk.org/about-cancer/ovarian-cancer/getting-diagnosed/screening on 08 July 2024.
- Cleveland Clinic. Ovarian Cancer. Accessed at https://my.clevelandclinic.org/health/diseases/4447-ovarian-cancer on 08 July 2024.
- American Cancer Society. Can Ovarian Cancer Be Prevented? Accessed at https://www.cancer.org/cancer/types/ovarian-cancer/causes-risks-prevention/prevention.html on 08 July 2024.
