Multiple Myeloma

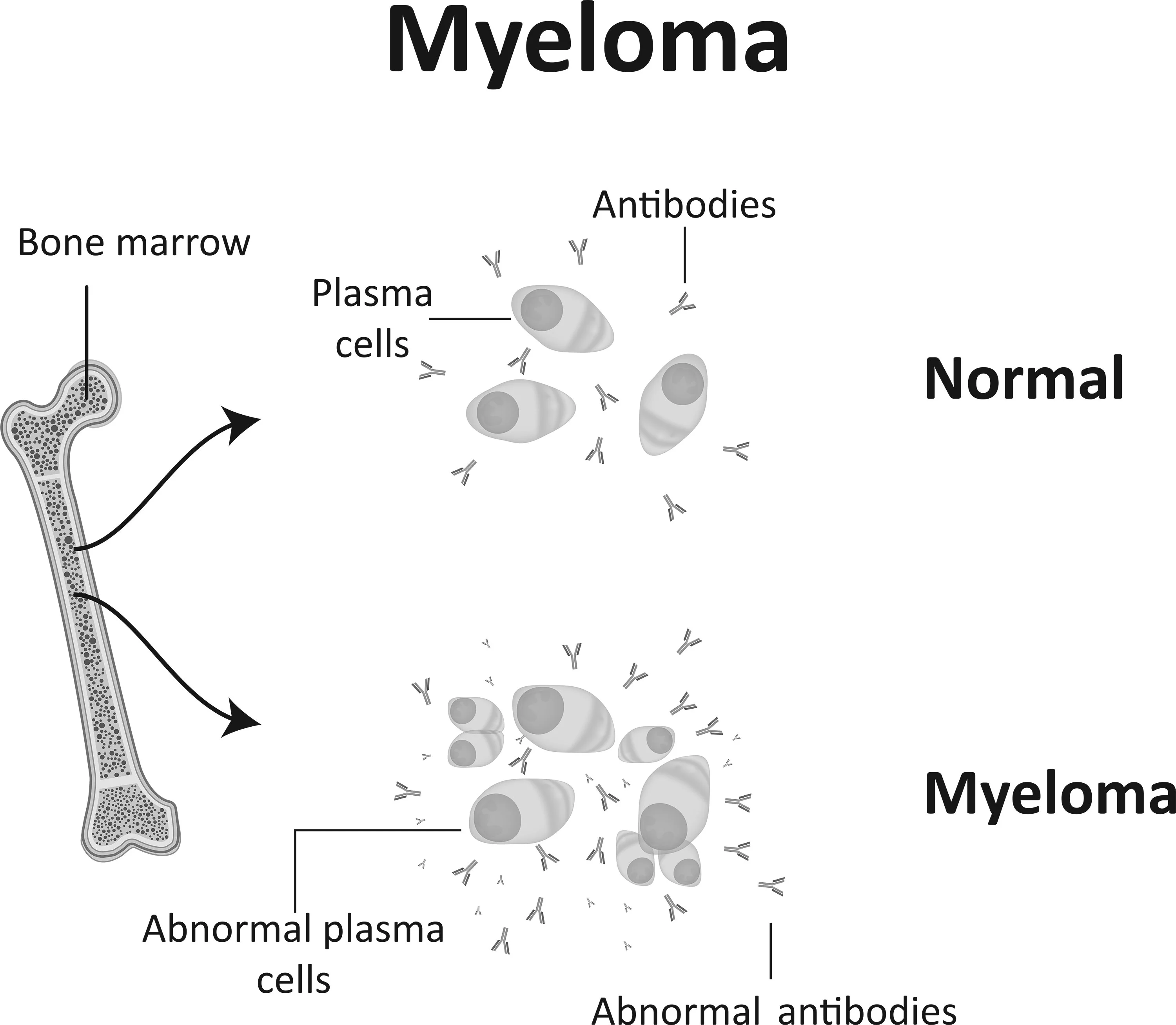
Multiple myeloma is a cancer of the bone marrow in which there is an uncontrolled production of malignant plasma cells in the body. In healthy people, plasma cells are white blood cells that normally produce antibodies to fight infections.
Myeloma cells accumulate in the bone marrow, preventing the bone marrow from producing healthy blood cells – oxygen-carrying red blood cells, infection-fighting white blood cells, and platelets needed for blood clotting.
In addition, myeloma cells produce non-functioning antibodies (called ‘M’ proteins) at an increased rate which, together with myeloma cells, can accumulate in several places in the body (hence “multiple” myeloma). The accumulation of these cause damage to vital organs and tissues including the kidney (causing kidney failure) and bone (causing fractures to easily occur as well as high calcium levels in the body).
The cause of multiple myeloma is not known. The following risk factors for multiple myeloma have been identified:
- Age – The risk of developing multiple myeloma increases with age. It is more common in people over the age of 65.
- Gender – Multiple myeloma occurs more frequently in men than in women.
- Race – African-Americans have a higher risk of developing multiple myeloma.
- Personal history – People who have had another plasma cell disease, Monoclonal Gammopathy of Undetermined Significance (MGUS), are more likely to develop multiple myeloma. MGUS is marked by the presence of M proteins in the body.
- Family history – The risk of developing multiple myeloma is higher for those who have a close relative (such as sibling or parent) with the disease.
- Obesity – Overweight and obese people may have a higher risk of developing multiple myeloma.
In the early stages, patients may not experience any symptoms of multiple myeloma. The symptoms may also vary from person to person. The common symptoms are:
- Fatigue
- Pale skin
- Breathlessness
- Weakness
- Nausea
- Increased thirst
- Loss of appetite
- Constipation
- Mental confusion
- Kidney damage
- Swelling in lower limbs (due to kidney problems)
- Frequent urination
- Bone pain or weakened or broken bones
- Pain in the back or belly
- Fever
- Frequent infections
There are various tests used to investigate and diagnose multiple myeloma, including blood tests, urine tests, bone marrow biopsy and radiological imaging (e.g. X-rays, MRI scan, PET-CT scan).
In the physical examination, the doctor will check for signs of disease, such as swelling or other unusual symptoms.
A full blood count is a blood test that involves a sample of blood being sent to the laboratory for investigation. The blood sample will be checked for the number of red blood cells, white blood cells and platelets. Further blood tests to check levels of abnormal M protein and other antibodies in the blood will also be needed.
Urine tests should also be performed at the time of diagnosis of multiple myeloma. These tests also check for the abnormal protein in the urine as well as amount of protein in the urine.
A bone marrow biopsy involves taking a sample of bone marrow, usually from the hip bone. This is done under local anaesthetic and takes 15 – 20 minutes. The sample will also be sent for investigation by the laboratory, to be examined for the number of myeloma cells, the karyotype and FISH tests (looking for abnormal myeloma chromosome changes).
Staging or determining the stage of cancer is helpful in deciding on treatment options. There are two systems for staging multiple myeloma: the Revised International Staging System (RISS) and the Durie-Salmon Staging System.
The RISS, which is commonly used, is based on four main factors:
- Amount of albumin in the blood – Albumin, a protein produced by the liver, is important in fighting infections and in the building and repairing of muscle tissue.
- Amount of beta-2 microglobulin in the blood – Beta-2 microglobulin is a protein produced by myeloma cells. High levels of this protein indicate an advanced stage of multiple myeloma.
- Amount of lactate dehydrogenase (LDH) in the blood – LDH is an enzyme found in tissues. High levels of this enzyme may indicate tissue damage.
- Specific gene abnormalities of the cancer (cytogenetics) – Certain chromosome changes, such as the loss of a piece of chromosome 17, have been linked to a poorer prognosis.
Based on the factors above, multiple myeloma is classified into three stages:
- Stage I: Serum beta-2 microglobulin is less than 3.5 mg/l; albumin level is 3.5 g/dl or greater; cytogenetics are considered “not high risk”; and LDH levels are normal.
- Stage II: Serum beta-2 microglobulin is between 3.5 mg/l and 5.5 mg/l; or albumin level is less than 3.5 g/dl.
- Stage III: Serum beta-2 microglobulin is 5.5 mg/l or greater and cytogenetics are considered “high risk” or LDH levels are high.
The Durie-Salmon Staging System was introduced in 1975 and updated in 2006. It is becoming less common for staging multiple myeloma because it does not account for the genetic (and chromosome) changes which are the most important prognostic factors in myeloma.
In the early stages of multiple myeloma, many people will not experience any symptoms (this is known as smouldering/ asymptomatic multiple myeloma) and will not need treatment. Patients will be actively monitored through regular check-ups and blood and urine tests. Treatment will usually begin only when the disease is more advanced.
Some of the standard treatment options are shown below. In general, combinations of 2-3 drugs are recommended for treatment of myeloma.
Targeted Therapy
In targeted therapy, drugs or other substances target specific cancer cells to destroy or block their growth, while leaving normal cells unharmed. For multiple myeloma, targeted drugs may be given that block myeloma cells from breaking down proteins, or that bind to myeloma cells, causing the myeloma cells to die. One of the most widely used drugs are called proteasome inhibitors, usually combined with immunomodulator drugs.
Immunomodulators
These are tablets that have high activity in myeloma and usually used in combination with proteasome inhibitors and steroids. Immunomodulators are also used alone after completion of proteasome inhibitor therapy as a way to maintain or control the growth/spread of myeloma cells.
Biological Therapy
Biological therapy drugs enhance the ability of the body’s immune system to identify and destroy myeloma cells. These are given by infusion through a vein (intravenous).
Chemotherapy
Chemotherapy uses drugs to destroy cancer cells or stop them from multiplying. The drugs may be given intravenously (through a vein in the hand or arm) or in tablet form.
Corticosteroids
Corticosteroids are important drugs in the treatment of myeloma. They are usually used in combination with other medications (as above). Corticosteroids may be given intravenously or in tablet form.
Radiation Therapy
In radiation therapy, high-energy X-rays are used to destroy myeloma cells in the body. External radiation therapy is provided by a machine outside the body. Radiation therapy may be used to quickly reduce the myeloma cells in a specific area, such as when abnormal plasma cells accumulate to form a tumour.
High-dose Chemotherapy with Stem Cell Transplantation
Younger patients (usually less than 65 years old) with myeloma should always be evaluated for suitability to undergo autologous stem cell transplantation. Autologous means that the stem cells are derived from the patient’s own body.
Autologous transplantation represents a highly important modality of treatment because of its ability to control myeloma disease for a more prolonged period. This kind of transplant is usually performed after a period of treatment with drugs(as above), when the myeloma cells have been mostly killed. The rationale is to give a high-dose of chemotherapy to kill whatever remaining myeloma cells there are and then to use pre-collected stem cells to rescue the patient’s bone marrow from the toxicity of high-dose chemotherapy.
As most of the risk factors for multiple myeloma cannot be avoided, there is no known way to prevent the disease.

CanHOPE is a non-profit cancer counselling and support service provided by Parkway Cancer Centre, Singapore. CanHOPE consists of an experienced, knowledgeable and caring support team with access to comprehensive information on a wide range of topics in education and guidelines in cancer treatment.
CanHOPE provides:
- Up-to-date cancer information for patients including ways to prevent cancer, symptoms, risks, screening tests, diagnosis, current treatments and research available.
- Referrals to cancer-related services, such as screening and investigational facilities, treatment centres and appropriate specialist consultation.
- Cancer counselling and advice on strategies to manage side effects of treatments, coping with cancer, diet and nutrition.
- Emotional and psychosocial support to people with cancer and those who care for them.
- Support group activities, focusing on knowledge, skills and supportive activities to educate and create awareness for patients and caregivers.
- Resources for rehabilitative and supportive services.
- Palliative care services to improve quality of life of patients with advanced cancer.
The CanHOPE team will journey with patients to provide support and personalised care, as they strive to share a little hope with every person encountered.
