Cervical Cancer

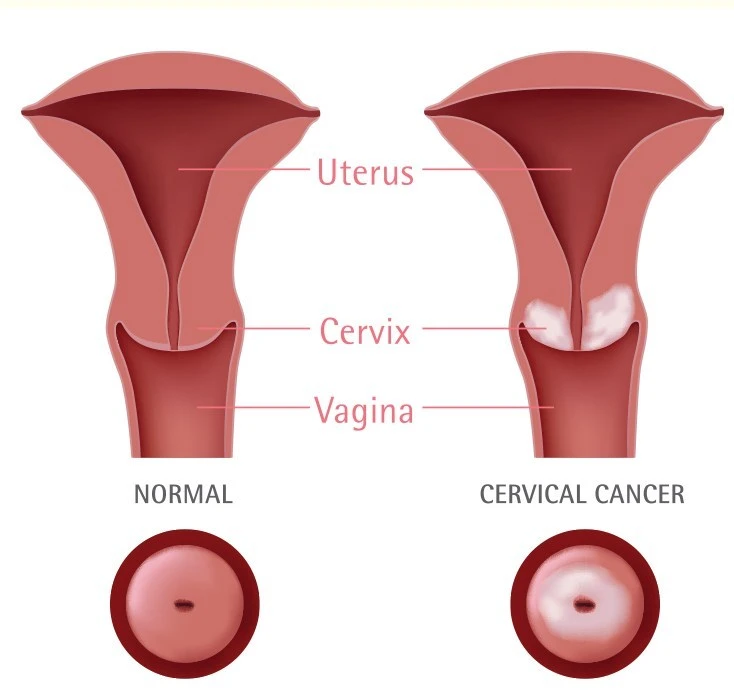
Cervical cancer is a disease in which malignant (cancer) cells form in tissues of the cervix (the organ connecting the uterus and vagina). There are many types of cervical cancer. The most common type, squamous cell carcinoma (SCC), constitutes about 80 to 85 per cent of all cervical cancers.
The other types of cervical cancer, such as adenocarcinoma, small cell carcinoma, adenosquamous, adenosarcoma, melanoma and lymphoma, are much rarer types of cervical cancer that are not generally related to HPV. The latter types of cervical cancer are not as preventable as SCC.
Anything that increases your chance of getting a disease is called a risk factor. Having a risk factor does not mean you will get cancer, not having risk factors does not mean that you will not get cancer.
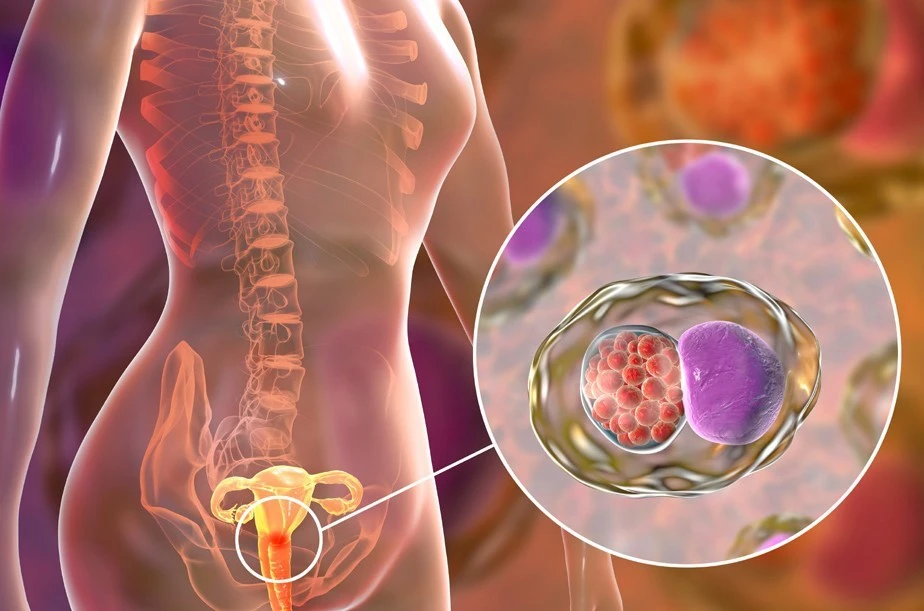
Human Papilloma Virus (HPV) infection is the major risk factor in the development of this cancer. These viruses are transmitted during sexual intercourse, as well as oral or anal sex.
All women who engage in sexual activity are at risk of developing cervical cancer. Some sexual behaviours, such as multiple sexual partners, having partners who have had multiple sex partners, and having sex at an early age further increase the risk. Other risk factors include:
- Cigarette smoking
- Long term use of oral contraceptives
- Have a weakened immune system which weakens the body’s ability to fight infections and other diseases. This may be due to infection with human immunodeficiency virus (HIV) or taking medicine to help prevent organ rejection after a transplant
- Having given birth to many children
Early cervical cancer may have no symptoms. You may experience the following symptoms:
- Vaginal bleeding
- Back pain/pelvic pain
- Pain during sexual intercourse, bleeding after sexual intercourse
- Abnormal vaginal discharge
- Painful or difficult urination or cloudy urine
- Chronic constipation and feeling of presence of stool despite having emptied bowel
- Leaking of urine or faeces from the vagina
While the Pap smear is an effective cervical cancer screening test, confirmation of the diagnosis of cervical cancer or pre-cancer requires a biopsy of the cervix. This is often done through colposcopy, a magnified visual inspection of the cervix aided by using a dilute acidic solution to highlight abnormal cells on the surface of the cervix. It is a painless 15-minute outpatient procedure.
Further diagnostic procedures include Loop Electrical Excision Procedure (LEEP), cone biopsies, and punch biopsies.
Cervical cancer usually develops slowly over time. HPV infection can cause the cells of the cervix to go through changes known as dysplasia, in which abnormal cells begin to appear in the cervical tissue. Over time, the abnormal cells may become cancer cells and start to grow and spread more deeply into the cervix and to surrounding areas.
CIN (cervical intraepithelial neoplasia) refers to lesions that do not invade the tissue of the cervix. It is at the superficial surface of the surface. CIN lesions are graded as I (mild), II (moderate) and III (severe). CIN III is a precancerous lesion.
It is important to note that not all ladies with HPV infections develop CIN, and not all ladies who have CIN develop cervical cancer. Many HPV infections are cleared rapidly by the immune system, just like any other infections.
Staging is a term that describes how far an invasive cervical cancer has spread. Stage I cervical cancer has invaded into the cervix, but has not extended outside of the cervix. Stage II cancer has spread to the upper vagina, or into the tissue to the sides of the cervix (the parametria). Stage III cancer has spread to the lower part of vagina and to the sidewall of the pelvis or has caused blockage of the kidney. Stage IV disease means that cancer has extended to other organs such as the bowel or bladder, or has spread to other organs such as the distant lymph nodes, liver, lung and bones.
Cervical cancer is treated with surgery, radiation therapy, chemotherapy, targeted therapy and immunotherapy. Depending on the stage and type of the cancer, you may need more than one type of treatment.
- Surgery
Surgery is often performed for early cervical cancer. The extent of surgery is dependant on the stage of presentation. - Radiotherapy
Radiation therapy is the use of high energy X-rays or radiation to kill cancer cells. It is often used in combination with chemotherapy to treat cervical cancer. - Chemotherapy
Chemotherapy are medicines which are either injected or taken orally to treat cancers. They enter the bloodstream and work by interfering with the ability of cancer cells to grow and divide. In cervical cancer, chemotherapy is often given with radiation to treat cancer that has not spread to distant organs. It is also used in treating cancer which has spread to other organs or tissues. - Targeted therapy
All cells including cancer cells need blood vessels to sustain and grow. By giving a treatment that targets against a protein that helps new blood vessels to form, cancer cells will not be able to grow and die. Targeted therapy is given with chemotherapy in the treatment of cervical cancer. - Immunotherapy
Immunotherapy are medications that harness the body’s own immune system and allow it to recognise and destroy cancer cells. Immunotherapy is a treatment option for cervical cancer which has come back (recurred), or has spread to distant organs.
Early cervical cancer usually have no signs or symptoms. However, it can be detected early with regular check ups. The earlier the detection, the higher the chance of successful treatment.
The Pap test, also called the Pap smear, is a cervical cancer screening test. This is done in an outpatient setting. The test is conducted by using a plastic or metal instrument, called a speculum, to widen the vagina. The doctor or nurse will then examine the vagina and cervix, and collect a few cells from the cervix and the area around it with a swab. These cells are then placed on a slide and sent to laboratory to be checked for abnormal cells. The high risk HPV (hrHPV) test can also be done on these cells to look for the type of HPV virus that causes cervical cancer.
Women should begin having cervical cancer screening at age 21, or within three years of first sexual activity – whichever happens first.
- If you are between 21 and 29, you should get a Pap test every 3 years
- If you are between 30 and 64, you should get a Pap test and HPV test together every 5 years or a Pap test alone every 3 years
- If you are 65 years or older, you can stop screening if prior cervical cancer screening results have been normal.
You can lower your risk of getting cervical cancer with the following steps:
- HPV vaccine have been developed that are effective against the strains of HPV responsible for 70 to 85 per cent of all cervical cancers. HPV vaccines are targeted at girls and women of ages 9-26 and works best before the start of their sexual activities.
- Get regular cervical screening test, even though one has had HPV vaccination. This will help detect and treat early changing cells that may turn into cancer.
- Alter sexual behaviour. Reduced exposure to HPV infection reduces risk of cervical cancer. Use condoms to prevent any sexually transmitted disease including HPV.

CanHOPE is a non-profit cancer counselling and support service provided by Parkway Cancer Centre, Singapore. CanHOPE consists of an experienced, knowledgeable and caring support team with access to comprehensive information on a wide range of topics in education and guidelines in cancer treatment.
CanHOPE provides:
- Up-to-date cancer information for patients including ways to prevent cancer, symptoms, risks, screening tests, diagnosis, current treatments and research available.
- Referrals to cancer-related services, such as screening and investigational facilities, treatment centres and appropriate specialist consultation.
- Cancer counselling and advice on strategies to manage side effects of treatments, coping with cancer, diet and nutrition.
- Emotional and psychosocial support to people with cancer and those who care for them.
- Support group activities, focusing on knowledge, skills and supportive activities to educate and create awareness for patients and caregivers.
- Resources for rehabilitative and supportive services.
- Palliative care services to improve quality of life of patients with advanced cancer.
The CanHOPE team will journey with patients to provide support and personalised care, as they strive to share a little hope with every person encountered.
